Beyond Nutrition: A Comprehensive Exploration of Obesity in Toddlerhood and Early Childhood
Prof. Antje Körner
Center of Pediatric Research, Dept. of Pediatrics, University Hospital for Children & Adolescents
Helmholtz Institute for Obesity, Metabolic and Cardiovascular Research, Helmholtz Munich
University of Leipzig, Germany
Obesity is a complex, chronic, relapsing and disabling disease. It has a high prevalence already in childhood with every 5th child being affected by overweight in Germany. For the first time in humankind, there are more children suffering from overweight than from underweight on a global level. Still, children living with obesity do not benefit from the scientific and clinical advance as adequately.
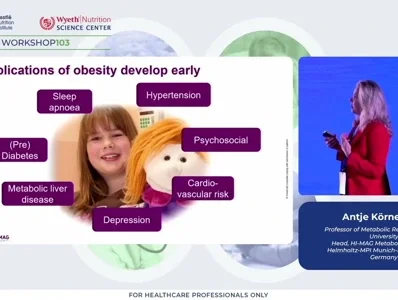
Early childhood between 3 and 6 years of age is a critical window for the manifestation of childhood obesity and once manifested, more than 90% of children with overweight will remain to have overweight into adolescence and beyond. Even though classical complications of obesity are diagnosed in adulthood, the development starts much earlier and already in childhood. However, we need better tools to detect the children at highest risk for complications. For example, metabolic parameters show clear dynamics over the life span, which is not reflected by current cut-offs. Applying age specific and insulin-based cut-offs enables a more precise and sensitive detection showing a 4-12-fold increased diabetes risk.
The causality of obesity is not as simple as just unhealthy nutrition and lack of physical activity. Obesity develops on the basis of a genetic predisposition, our biology regulating energy balance always to defend energy reserves integrated by the brain, and this hits our Western life style. So nature and nurture interact in the development of obesity.
Evidence for the environmental impact comes from studies during Covid associated lockdown with profound effect on our health behavior or the association of the built environment of a childs surrounding and health behavior and medical issues including obesity.
The strongest risk factors for childhood obesity on an epidemiological level are parental overweight, low socioeconomic status followed by early life factors. For example, a high birthweight is risk factor for obesity in early childhood and the risk for high birthweight is driven by maternal obesity and in addition weight gain during pregnancy. But also obesity in the father can drive obesity and metabolic risk in the offspring due to epigenetic molecular sperm-mediated effects. Early life nutrition can also affect adipose tissue biology, for example breast-milk derived lipid species can pertain brown adipose tissue. Also environmental pollutants can affect adipose tissue biology.
Regarding the genetic predisposition, we need to differentiate between common polygenic predisposition based on a huge multitude of genetic variants, which alone have minimal effect size and the functional basis is often not known. On the other hand there are rare monogenic obesity forms, usually with mutations in genes implicated in the central hypothalamic energy regulating circuits. Nevertheless, it is important to detect these variants and the patients as there are now treatment options available.
Overall, obesity develops based on a genetic predisposition and our exposure to multiple exogenous risk factors. We need to identify the patients at highest risk for early progressive disease courses and complications and to understand the mechanisms behind these associations to develop more precise and targeted treatment and prevention approaches to overcome the treatment gap.