Update: Allergies and the intestinal microbiome
Successes in allergy prevention
The risk of developing allergies is significantly shaped by early life influences. In addition to the disposition, the type of delivery, duration of breastfeeding and the selection of the supplementary foods are the greatest influential factors.
Breast milk also reduces the risk of a series of non-transmissible diseases, including allergic conditions. If one cannot breast feed, an infant formula as similar as possible
to breast milk is very important.
Cow milk-based formula contains cow milk proteins, which represent a risk factor for allergic sensitization and atopic eczema in infants with increased risk of allergies. A hydrolyzed formula contains cow milk protein, which is partially or completely broken down (hydrolyzed). Depending on the degree of hydrolysis, one speaks of partial (= pHF) or extensive (= eHF) hydrolyzed nutrition.
The GINI study, the largest state funded long-term study on the prevention of allergic conditions in children with an increased allergy risk has resulted in significant knowledge about long-term health effects of early prevention. It shows that even partially hydrolyzed nutrition can reduce the risk for atopic eczema in the first year of life by 50 percent compared to non-hydrolyzed. Participants in the GINI study have been observed for more than 20 years. The most significant results:
- Risk reduction of atopic dermatitis in the first year of life by 50%
- The preventative effect on atopic dermatitis remains into adulthood without rebound.
- Also reduction of the risk of asthma after puberty
But every HA formula is unique with regard to its peptide profile. Not only the base protein and the degree of hydrolysis, but also the hydrolysis process plays an important role for efficacy. The hydrolysis process not only influences the size of the peptide, but also directly the sequence of the various amino acids. The sequence plays a key role in the ability of peptides to induce immune tolerance.
Not or not only breast fed infants, whose parents or siblings are affected by an allergy should receive a hydrolyzed formula (HA formula) in the first year of life, for which the preventative efficacy has been proven - Ernährungskommission der DGKJ, 2018
Literature Sources
Would you like further information on the topics discussed? You will find the detailed source information for the articles in this issue on the NNI website.
Mechanisms of an allergy tolerance
Oral tolerance is the non-reaction with absorbed allergens. A food allergy arises when no oral tolerance is developed, which usually occurs in infancy and early childhood.
The first contact with food allergens primarily occurs via the gastrointestinal tract or skin, and may occur in various prenatal and postnatal phases. An additional path of allergic sensitization may occur via the respiratory tract tissue. Due to the immaturity of their intestinal barriers and their immune systems, infants and small children are particularly vulnerable.
Currently there are no effective strategies to build up a permanent tolerance. Recent findings point to the protective effect of early contact with peanuts and eggs in children with eczema. Skin rashes may be countered with oral tolerance. An additional approach is the restoration of the skin barrier in high-risk children.
The treatment of food allergies consists of recognizing the adverse reactions and consequently avoiding the triggers.
Nowak-Wegrzyn A, Chatchatee P: Ann NutrMetab 2017 – DOI: 10.1159/000457915
Alleviating allergy risks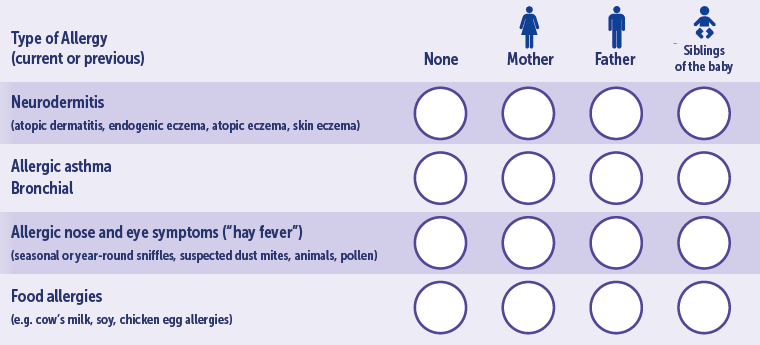
If there are already allergies in closerelatives (parents, siblings), there is an increased risk to the baby of also developing an allergy. The possibility can be detected even during pregnancy with a simple questionnaire. This helpful questionnaire should be used in consultation and can be downloaded at:
https://germany.nestlenutrition-institute.org/hebammen/arbeitsmaterialien
A new generation of therapeutic nutrition
Cow milk proteins (CMP) are some of the most frequent food allergens in infancy. Avoidance in foods is the most important measure to treat cow milk allergies. If breast-feeding is not possible, tested hydrolyzed infant formulas are recommended.
The new generation of hydrolyzed infant starting formulas - extensively hydrolyzed formula on a milk base (w-eHF) and amino acid-based infant formula (AAF) - contain oligosaccharides (HMO), which are structurally identical to the relevant HMO in breast milk.
HMOs act as prebiotics, among other things, and serve as nutrients for non-pathogenic bacteria (e.g. bifidobacteria), which they transform into short-chain fatty acids for the tolerance of allergens. HMOs act as “bait” for pathogenic bacteria by limiting their access to the intestinal epithelium.
The first studies on healthy infants revealed that the infant formulas with two HMOs, 2’Fucosyl-Lactose (2’FL) and Lacto-N-Neotetraose (LNnT) were well tolerable and supported normal growth. IN addition it was proven, that the formula with 2’FL and LNnT was associated with a reduction of infections as well as the use of antibiotics and fever-reducing medications in the first year of life compared to infant formula without HMO. There was also a positive modulation of the intestinal microbiome. These studies substantiate the safety and efficacy of the novel hypoallergenic w-eHF with 2’FL and LNnT in infants with a cow milk allergy.
Nowak-Wegrzyn A: WCPGHAN 2021
Do cats help asthma?
Cats and dogs may reduce the risk of asthma in childhood if a certain genotype is present, as shown by an investigation by the Copenhagen Prospective Studies on Asthma in Childhood2000 (COPSAC).
In 377 children with an increased risk, the interaction was determined between the exposure to cats/dogs and the chromosome 17q21, the strongest known genetic risk factor for asthma. The primary end point of the study was the development of asthma until the age of 12 months.
The exposure to cats and/or dogs from birth on was associated with a lesser prevalence of asthma in children with the rs7216389-high-risk-TT genotype, however without effect in children with the CC/CT genotype, which shows an interaction between cat and dog exposure and the rs7216389 genotype. The exposure to dog allergens showed no such interaction. This indicates that an early childhood exposure to cats reduces the risk of asthma, pneumonia and bronchiolitis in genetically susceptible
persons.
Stokholm J et al.: J Allergy Clin Immunol 2018
Amino acid formula supplemented with HMO: Tolerability and safety
Can an amino acid formula (AAF) supplemented with two human milk oligosaccharides (HMO) be well tolerated by infants with a cow milk protein allergy (CMA) and support normal growth? This was investigated by a study in 6 pediatric institutions in Australia.
Infants from 1-8 months with moderate to severe CMA took part, in whom trials with extensively hydrolyzed infant formula (eHF) or rice-based infant formula failed and who required AAF as a first line treatment. The study was about a an AAF supplemented with two HMOs, 2‘Fucosyl-Lactose (2‘FL) and Lacto-N-Neotetraose (LNnT). The infants received the formula for 4 months and as needed up to an age of 12 months. From the 4-6th month, the infants received supplementary food free of cow milk proteins. Weight, length and head circumference were measured monthly from inclusion in the study (V0) to the 4-month follow-up (V4) and at an age of 12 months (V5). The tolerability and safety were assessed using the adverse events reported during the study.
Infants with moderate to severe CMA achieved a normal growth with a certain catch-up growth with the HMO study formula. Except for a small number of non-severe gastrointestinal side effects, the formula was well tolerated and displayed outstanding safety.
Gold MS et al: EAACI Hybrid Congress, July 2021
INTERVIEW - "Breast milk protects in various ways"
Prof. Michael Abou-Dakn - Medical Director at St. Joseph’s Hospital Berlin Tempelhof and Chief Physician of the Clinic for Gynecology and Obstetrics, Professor of Obstetric Medicine in Midwife Studies at the Evangelical University of Berlin as well as Member of the National Breast-feeding Committee.
Professor Abou-Dakn, why and how should allergy prevention begin as early as in pregnancy.
Today we know that even in pregnancy on the part of the mother, allergic reactions can be promoted in the child. We have information on what the
biochemical processes are that then later trigger allergies. It appears that the non-infectious diseases in children, such as asthma, diabetes, obesity and even allergies can be contracted as early as during pregnancy, but also during birth, vaginally or by
cesarean section.
Breast milk is thus ideally suited for the nutritional needs of the infant in the first months of life. Apparently it also provides protection against infectious diseases and allergies, is that so?
Yes, and in a varied manner. On the one hand through various proteins which can actually actively prevent infection, thus the so-called nest-protection, that is created both during pregnancy via the mother hen as well as via the mother’s milk itself.
We know from many diseases that the mother can not only provide these specific proteins, these antibodies, but that there are also unspecific functional elements that, on a general level, very quickly prevent the disease pathogens being transferred at all, or if they do reach the child, do not enter the child’s system. So, for example, if probiotics are present via the intestinal flora that prevent bacteria entering the child’s intestinal mucous membrane and which then could cause an illness. This is indeed a special phenomenon. Because apparently the composition of this combination of active agents changed in the mothers during the breast-feeding period or if they themselves are ill. This means that each child receives targeted individual protection. This also varies with premature births. Because there too the composition of the mother’s milk adapts individually to the special need, that’s wonderful.
Except for a significant strain, the mode of birth and certain environmental influences, does the type of nutrition influences the risk of developing an allergy?
Nutrition of course also plays a great role. On the one hand in the feeding of the child: With the introduction of supplemental food, the child comes into contact with a series of elements that could lead to allergies. In our breadth, the peanut contact was less frequent, but in America it plays a large role as the most frequent trigger of a food allergy. Even cross allergies must be considered, such as with birch there is relatively frequently a cross allergy to pomaceous fruit. Therefore it is clear that there may be allergic reactions via the ingestion of foods.
For allergy prevention, is a tolerance development through early contact recommended instead of stricter avoidance?
Today we know that the introduction of foods after breast-feeding is such that one should not avoid them, as previously recommended. With allergies one must understand, that they are an overreaction to antibodies. A successive adjustment prevents this severe reaction.
However, it appears to be very important that breast-feeding is still provided when women slowly introduce their children to solid foods in this phase. From studies with mice, we now know exactly that substances are present in breast milk that prevent allergy development.
In this, the colonization of the early childhood intestinal microbiome, also called intestinal flora, plays a decisive role.
Today we know that the variety of germs from pathogenic and positive bacteria play an important role in the protection from allergies and that therefore a balanced and rich intestinal flora is very good. We also know that with a cesarean section, there is no effect on the maternal germs, because it
is an aseptic environment, which is not conducive to nest protection.
Breast-feeding is also very important for the child’s microbiome because we are gaining knowledge that the mother’s milk is also influenced by the maternal intestinal flora. Partially because there are sufficient certain bacteria that contribute to the development of a favorable microbiome in the infant.
One must take into consideration that infections of the breast are also reduced, such as mastitis. There is also apparently a connection between the maternal intestine and the the mammary glands.
For the interaction of “good” and “bad” bacteria, is one component of the breast milk of great importance, the so-called human oligosaccharides, HMOs for short?
The HMOs are prebiotics that are made available individually in great variety. These are certainly one of the significant factors that increases the infection and allergy protection for children. It is very interesting how the composition of the breast milk adjusts to the relevant situation accordingly.
However, do the occurrence and the composition of the HMO differ from woman to woman? Which factors are responsible for this?
There is a very colorful pattern, and these apparently associated with genetics and the situation of the mother. Because the HMOs are also changed. There are HMOs that are very regularly found, but here even more individuality is created. But it is not surprising, because we know today that stem cells are also transferred via breast milk. There is an deep interaction between the health of the mother and that of the child.
Do first results show that for the treatment of food allergies, the HMO supplement to a formula based on amino acids promises success?
Yes, that it what we are expecting. Because ultimately it is about the conflict with certain substances which can be quasi encased in this way. Thus they prevent them being recognized as an allergen at all. Or the intestinal flora is armed with antibodies so that no rapid overreaction occurs. Thus one can imagine that HMOs are effective against existing food allergies. It is ultimately about the development of a healthy microbiome in the child.
Action of human milk oligosaccharides
Human milk oligosaccharides (HMOs) are extensions of the milk sugar lactose with galactose, N-acetylglucosamine, fructose and sialic acid. Clinical observation studies with breast-fed infants and mothers connect specific HMOs with the intestinal microbiome of the infant and its healthy development.
Observation data and data from the fundamental research indicate that HMOs influence the establishment of the microbiome and the mucous membrane immunity in early life and inhibit pathogens, thus contributing to protection from infection. Clinical intervention studies with a formula supplemented with a single HMO, 2’-Fucosyllactose (2’FL) or with two HMOs - 2’FL and Lacto-N-neotetraose (LNnT) have shown that it enables age-appropriate growth and is well tolerated.
The data connected the feeding with a formula with 2 HMOs with less reported diseases of the upper respiratory tract and a lesser need for antibiotics during the first year of life, compared to feeding with a control formula. Parallel to this, the composition of the microbiome shifted in the first year toward that of nursed infants. Taken together, HMOs probably contribute partially to immune protection. These results justify further clinical research to deepen the understanding of the biology of the HMOs and their significance for the nutrition of infants.
Sprenger N, Binia A, Austin S: Nestle Nutr Inst Workshop Ser 2019 –DOI: 10.1159/000490292
The microbiome from infancy to early childhood
The establishment of the gastrointestinal microbiome in infancy influences the development of the immune system and oral tolerance induction. The birth mode and nutrition can contribute during this period to the development of immune-mediated diseases.
1453 stool samples from 440 children (49.3% girls, 24.8% born by cesarean section; all children except for 6 were nursed for varying periods) were taken 5, 13, 21 and 31 weeks after birth and once at school age (6-11 years) and the microbiome analyzed from them. The development of atopic dermatitis was observed until an age of 3 years and data about allergic sensitization and asthma were collected at school age.
The diversity of the fecal microbiome did not vary significantly among the children from 5 to 13 weeks after birth, but increased thereafter to 21 and 31 weeks. The greatest increase in the microbial diversity occurred after 31 weeks. A vaginal delivery was associated most strongly with an enrichment of bacterial species between 5 and 31 weeks compared to a cesarean section. From the 13th week, nutrition becomes the most important factor in the microbiome composition. The end of breast-feeding and not the introduction of solid food was associated with changes. It has been shown that the composition of the fecal microbiome is connected to the development of atopic dermatitis, allergic sensitization and asthma.
Galazzo G et al. Gastroenterology. 2020 – DOI: 10.1053/j.gastro.2020.01.024
Early influential factors on the intestinal microbiome
The development of the intestinal microbiome of each infant is influenced by many environmental factors, including geography, family, family structure, pets and antibiotics in addition to genetic and maternal factors. By far the most important is the type of birth (cesarean section versus vaginal delivery) and the type of nutrition (breast-feeding versus formula).
Breast-feeding promotes the development of a microbiome with significant diversity and the predominance of specific species, in particular bifidobacteria and lactobacillae through multiple mechanisms, including the composition of the breast milk bacteria and oligosaccharides in the breast milk. Breast-fed infants generally have a lower risk of infection and immunological diseases such as asthma, other allergies, type 1 diabetes and leukemia as well as metabolic diseases.
This is similar with a vaginal delivery. After a cesarean section there was a less diverse microbiome and changed microbial profile, including a lower presence of bifidobacteria. Increasingly, strong associations have been reported between cesarean section delivery and diseases in infancy and later in life. However, a birth by cesarean section increases above all the risk of allergic diseases, including asthma, atopic dermatitis and food allergies.
When using specific species and strains of bifidobacteria and lactobacillae as probiotics, it has been shown that they have effects on infectious intestinal and respiratory tract diseases as well as on the modulation of the intestinal barrier function, IgA secretion and the activity of T-lymphocyte modulation.
Saavedra J: The Nest 48, 2021
Advantages for the intestinal microbiome of the infant
There is evidence that oligosaccharides (HMO) offer numerous advantages for infants, including prebiotic effects, intestinal maturation, antimicrobial activities and immune modulation.
The effects were examined of an infant formula with HMO 2’-Fucosyllactose (2’-FL) on biomarkers of the immune function within the framework of a randomized, double-blind, controlled growth and tolerance study in healthy full-term single children (birth weight an average of 2490 g) until an age of 4 months, who either received exclusively formula (n =317) or were breast-fed (n = 107). The infants who were fed formula randomly received 1 of 3 formulas that all contained 2.4 g total oligosaccharide/L.
- Trial formulas: GOS + 0.2 or 1.0 g 2‘-FL/L
- Control: only galacto-oligosaccharides (GOS);
- compared to a nursed reference group.
Blood samples were taken at the age of 6 weeks.
Nursed infants and infants who were fed one of the two study formulas with 2’-FL had no differences, but had 29-83% lower concentrations of inflammatory cytokines in the plasma than the infants who received the control formula. Infants fed with 2’-FL displayed lower plasma and ex-vivo inflammatory cytokine profiles that were similar to a nursed reference group.
Goehring KC et al.: J Nutr 2016
“Mama has superpowers”
This year’s Swiss Nursing Campaign is primarily targeted toward working mothers who wish to continue to nurse their babies after maternity leave. The numerous advantages of breast-feeding were presented in inserts, flyers, online banners and blogs and support offered for re-entering the workplace. The campaign also has the objective of sensitizing employers to the needs of nursing mothers. Because successful breast-feeding is not only dependent on the mother alone, but on her entire environment. Pregnant women and new mothers can find additional valuable advice on breast-feeding at www.stillkampagne.ch.
Changes to oligosaccharides in breast milk
Human milk oligosaccharides (HMOs) are important functional biomolecules in breast milk. But differences in the HMO composition and changes in its concentrations while-breast-feeding should be observed.
An overview summarizes the total and individual concentrations of HMO from the data, published from 1999 to 2019. The studies show that the HMO concentrations in colostrum are the highest (average 9-22 g/L). Somewhat lower concentrations are present in the transition milk (average 8-9 g/L), with a gradual regression in mature milk with advanced lactation, from 6-15 g/L in breast milk, which was collected within one month after the birth, to 4-6 g/L after 6 months. Significant differences in HMO composition was described among individual countries. It has been shown that various HMOs prevail during lactation, e.g. 3-fucosyllactose increases during lactation, while 2’-fucosyllactose decreases.
Thum C. et al.: Nutrients. 2021 – DOI: 10.3390/nu13072272
While lactose and HMOs are the typical carbohydrates in the firstmonths of life, the carbohydrate profile is expanded with the introduction of solid foods.
“Breast Crawl” at the first taste
The first hours after birth are decisive for easing the start of breast-feeding.
Even shortly after birth, the baby can intuitively find its way to its mother’s breast. Immediately after the birth, the infant first needs a period of rest, then small movements with the head and shoulders occur as well as the first mouth and sucking movements, all laying on its stomach on the mother’s stomach. Undisrupted contact and patient are necessary: After about an hour, the baby has reached the nipple, independently latched on and started to suckle.
Science calls this phenomenon Breast Crawl, when the newborn independently and single-mindedly finds its way to the breast. Each child has their own tempo. Medications administered during the birth, such as due to peridural anesthesia (PDA) can delay this breast crawl a bit.
www.gesund-ins-leben.de/fuer-familien/fit-durch-die-schwangerschaft/fru…
The microbiome of the pregnant woman influences the child’s behavior
An increased diversity of the intestinal microbiome of the mother during the third trimester of pregnancy can influence the brain development and behavior of the child, as reported by a new study from Australia.
The data of 213 mothers and 215 children who took part in the Barwon Infant Study (BIS) were analyzed, and the behavior of the children aged two years
observed using the Child Behavior Checklist. The connection between a higher maternal percentage of the butyrate producers lachnospiracae and ruminococcaceae (including most butyrate producing bacterial strains) and children with improved behavior is consistent with the increasing evidence that butyrate is neuroprotective.
The results support the knowledge from animal studies and indicate that during pregnancy there is a developmental window in which aspects of
the maternal prenatal intestinal microbiotics influence brain development in the fetus and thus also the behavior of the offspring.
Dawson SL et al.: Lancet EBioMedicine, 2021 – DOI: https://doi.org/10.1016/j.ebiom.2021.103400
Update on guideline on food allergies
The existing guideline on immunoglobulin-E (IgE) related food allergies from the year 2015 was updated by multiple specialists after a literature search, meta analyses, clinical studies and other scientific investigations.
The consensus of the review was achieved by an interdisciplinary committee of experts. It took into consideration the methodical specifications of the working group of the Scientific Medical Professional Societies (AWMF) for the development of guidelines for diagnostics and treatment and is consistent with an S2k guideline.
The most important recommendations are summarized:
- During pregnancy and lactation, a balanced, varied diet that covers the nutrient requirement is recommended. This includes consumption of vegetables, milk/milk products, fruit, nuts and eggs and fish.
- There should be no dietary restrictions (avoiding possible food allergies) during pregnancy or while breast-feeding.
- Breast-feeding has many advantages for the mother and the child. If possible, one should breast-feed exclusively for the period of the first 4–6 months.
- Breast-feeding should continue with the introduction of solid foods.
- If one cannot or cannot sufficiently breast-feed, formula should be used. One must check for risk children whether a formula with effective allergy prevention proven in studies is available until the introduction of solid foods.
- Soy-based formulas are not suitable for allergy prevention and should not be used for that purpose. Because there is no evidence of an allergy-prevention effect with other animal milks, such as goat, sheep or mare’s milk, these should also not be used for allergy prevention.
- There is no recommendation on the administration of prebiotics and probiotics for allergy prevention.
- Depending on the disposition of the infant, feeding solid foods should start at the earliest from the beginning of the fifth and at the latest from the beginning of the seventh month.
- There is no evidence of a preventative effect of dietary limitations by avoiding potential sources of food allergies in the first year of life. This should therefore not occur.
Worm M et al.: Allergologie 2021 – DOI 10.5414/ALX02257
Omega-3 fatty acids during pregnancy
Fatty seafood above all provides valuable omega-3 fatty acids. This also includes docosahexaenoic acid (DHA), which is important for the normal development of the child. DHA is a long-chain omega-3 fatty acid, which the human body can form on its own from precursors only in a limited manner. DHA is also important for brain function and vision. Even the unborn child requires sufficient DHA so that capacities such as thought processes and vision can develop well.
If one does not want to eat fish, targeted nutritional supplements can ensure DHA provision. For example using DHA enriched plant oils, according to the recommendation of the “Into A Health Life” network at the Federal Center for Nutrition.
Omega-3 fatty acids can promote the brain and vision of the baby
A Finnish study examined the connection between the maternal diet and the serum fatty acids during pregnancy and brain development in early infancy and childhood.
Infants whose mothers ate fish three or more times a week in the last trimester fared better than those whose mothers ate no fish or only up to two portions of fish per week. The results indicate that frequent fish consumption by pregnant women is an advantage for the development of their unborn child. This could be traced back to the long-chain polyunsaturated fatty acids (LC-PUFAs) in the fish, but also to other nutrients such as vitamin D and E, which are also important for development. LC-PUFAs contribute to the formation of the nerve cells, which are important for the retina as well as for the formation of the synapses which are essential for the transport of information between the neurons in the nervous system.
Normia J et al.: Pediatric Research 2019
B12 absorption and childhood development
Nutrient-deficiency in pregnancy is disadvantageous for the development of the fetal brain, which can lead to an affectation of cognitive function in childhood.
For a British study, longitudinal data from over 10,000 children born in 1991/1992 were used to clarify whether a prenatal vitamin B12 deficiency is damaging to the developing fetus.
Children of women with the lowest B12 consumption of 10% had:
- an increased risk for poor vocabulary at 24 months,
- reduced capacity of combining words at 38 months,
- poor speech comprehension at 6 years,
- poor mathematical comprehension in school years 4 and 6 (aged 8–9 and 10–11 years)
- poor results in national mathematics tests (aged 13).
There are no such significant adjusted association for reading or writing abilities or for the verbal or complete IQ (Intelligence Quotient) at 8 or 15 years. Low vitamin B12 consumption during pregnancy thus has negative effects on the development of the child.
Golding J et al.: Nutrition Research, 86, 2021
The consequences of poor iodine levels in pregnant women
More and more young women have an increased risk that their children will be born with neurological affectations due to insufficient iodide. Dietary trends, the increasing eschewal of bread and iodized salt, as well as a low consumption of animal products containing iodine may contribute to a low iodine level.
In a pilot study by the University of South Australia (UniSA), in which 31 vegan/vegetarian participants and 26 omnivores were compared, there were iodine values of 44 ug/L in the vegetal group, compared to 64 ug/L among the meat eaters. Participants in both groups who used pink salt or Himalayan salt instead of iodized salt, has a significant iodine deficiency on an average of 23 ug/L. The value of 100 ug/L recommended by the WHO was achieved in none of the groups.
During pregnancy, the iodine requirement is increased and it is recommended to ingest 150 mcg (in Germany 230 mcg) before conception and during the entire pregnancy. Unfortunately most women do not take iodine supplements before conception. It is important to ensure sufficient iodine intake, in particular during the child-bearing years. It has been shown that a slight to moderate iodine deficiency affects the speech development, memory and the mental processing speed. Iodine sources in the diet include enriched bread, iodized salt, seafood including algae, eggs and milk products. Milk on a vegetable basis has a low iodine content.
The vegan/vegetable group also did not achieve the recommended values for selenium and B12 without supplements, but their intake of iron, magnesium, vitamin C, folic acid and dietary fiber was higher than the meat eaters. This reflects the intake of iron-rich soy products, whole grain products, pulses and green leafy vegetables in their diet. A US study from 2017 revealed that nearly two billion people around the world have an iodine deficiency, which leads in 50 million to clinical side effects.
Whitbread JS et al.: International Journal of Environmental Research and Public Health, 2021 – DOI: 10.3390/ijerph18073547
Lactose intolerance?
People who do not tolerate milk suffer from lactose intolerance. Important: This is a metabolic disorder and not an allergy.
The enzyme lactase, necessary for the digestion of lactose contained in the milk, is missing or it has very low activity. Thus the lactase enters the colon undigested, where intestinal bacteria convert it into acids and bloating gases. This can lead to diarrhea, cramping and other digestive problems. Despite this, one does not have to avoid milk and dairy products completely. Because depending on the processing, they contain more or less lactose.
www.in-form.de/wissen/lebensmittel-unvertraeglichkeit0/
Professional advice requested
The first year of life is a unique time in which parents or caregivers have to make all of the significant dietary decisions. They get good advice from all sides, including from the internet, but these are often not consistent with professional recommendations.
Parents expect individual instructions on infant formula from midwives, doctors and pediatric nurses. Studies show, however, that many parents think this professional dietary advice is insufficient. This could be due to the usually short consultation times, or that the consultation did not sufficiently take into consideration the importance of dietary questions for the parents or the influence of cultural and regional eating habits.
After birth, frequent visits are of fundamental importance for a continual dietary consultation consistent with the guidelines. Such as continuing to breast-feed and, if this is not possible, the use of suitable formula. Notable is the frequent use of whole milk as a replacement for breast-feeding on the advice of the family, and its negative effects. The introduction of solid foods is of great importance.
Feferbaum R: The NEST 47, 2021
The intestinal microbiome in premature babies
Breast milk is the most important factor for the development of the microbiome until an age of 12 months. One of the main tasks of oligosaccharides in breast milk is serving as a prebiotic, in particular for bifidobacteria.
Using 1477 stool samples from healthy premature babies, the clinical variables associated with the intestinal microbiome were examined. It is surprising that the gestational age and the birth weight are not significant factors for the microbiome profile. Much more significant were antibiotics, breast milk and breast milk supplements, while prebiotics were most strongly associated with a change in microbiome development.
Stewart C: 96th Nestlé Nutrition Institute Workshop, 2020
Oligosaccharides in the breast milk of preterm births
Oligosaccharides (HMOs) are a main component of the breast milk and play an important role in the protection of the infant from infections. Preterm babies are particularly at risk, but have a better protection if fed with breast milk.
A study examined whether the HMO composition of premature born mil of these deviates from breast milk in the same lactation phase and same gestational age. 22 HMOs in 500 milk samples from 25 mothers were analyzed, who were nursing preterm babies (< 32 week of pregnancy, < 1500 g birth weight), and 28 mothers who were nursing fullterm babies. The concentrations of the most HMOs were comparable at the same postpartum age. At comparable gestational ages, the concentrations of a series of HMOs in preterm birth milk differed significantly from that of full-term babies. The greatest differences occurred around the 40th week of post-menstrual age, when the milk of full-term babies contains the highest HMO concentrations.
Austin S et al.: Human Milk Oligosaccharides in the Milk of Mothers Delivering Term versus Preterm Infants. Nutrients 2019– DOI: 10.3390/nu11061282
A possibility of NEC prevention?
Bifidobacteria are the most frequent bacteria in the gastrointestinal tract of nursed full-term infants. In preterm infants, there is a significant connection between the composition of the intestinal microbiome (presence of clostridium neonatale can the lack of bifidobacteria) and the occurrence of necrotizing eneterocolitis (NEC).
It has been shown that the milk of mothers of preterm infants has a significantly lower content of 2‘-Fucosyllactose (2‘-FL) than that of mothers of full-term infants. The addition of two human milk oligosaccharides (HMOs), 2‘-FL und Lacto-N-Notetraose (LNnT), to formula leads to an alignment of the intestinal microbiome to that of
the nursed infant.
A current French study should now prove the effect of a liquid nutritional supplement in preterm infants that contains two HMOs, 2’-FL and LNnT.
Hascoët J-M: Microbiota And HMO In Preterm Infants. 96th Nestlé Nutrition Institute Workshop, 2020
Omega-3 supplementation against preterm births
Nutrients contribute to a number of mechanisms that may be important for a preterm birth. Dietary interventions offer a possibility for prevention.
Randomized studies on the effects of supplementation with zinc, micronutrients such as iron and folic acid as well as vitamin D are promising, but the results have been contradictory. The strongest evidence for a dietary solution to date has been the longchain polyunsaturated fatty acids (LC-PUFAs). Analyses of the ORIP study (Reduce the Incidence of Prematurity) revealed that women with low omega-3 overall status have a higher risk for very small early preterm infants (EPTB) which was significantly reduced through omega-3 supplements. Contrary to this, women with high overall omega-3 status already had a low EPTB risk. An additional omega-3 supplementation increased the EPTB risk compared to the control group.
These results show that the determination of the PUFA status of an individual woman could be the most precise way to implement recommendations to reduce the risk of preterm birth.
Conclusion:
- Diet-specific interventions can offer a promising solution to reduce the number of the nearly 15 million preterm births per year.
- The strongest evidence to date for dietary intervention is present for long chain polyunsaturated omega-3 fatty acids.
- Women with low omega-3 levels in early pregnancy could profit from a nutritional supplement.
- The determination of the individual status of the polyunsaturated fatty acids of a woman in early pregnancy could be an important path for recommendations to reduce the risk of preterm birth.
Best KP, Gomersall J, Makrides M: Ann Nutr Metab 2020 – https://doi.org/10.1016/j.nutres.2020.12.005
Breast-feeding is the optimum for preterm babies.
According to the guidelines of the American Academy of Pediatrics, all preterm infants should be fed on their mother’s milk or donor milk, if no milk is available from the mother. Donor milk does not contain enough proteins and other nutrients for appropriate growth of preterm infants, so it must be enriched. In addition, during pasteurization many important bioactive components of breast milk are lost and the majority of the living microbes in the donor milk are destroyed.
Feeding with breast milk contributes to the development of the intestinal microbiome of the infant, but recent studies show that the first colonization of the infant intestine can already start in the mother’s womb. Even the type of delivery affects the development of the early intestinal microbiome. The use of antibiotics in pregnant women and preterm infants also has an effect.
The provision of breast milk cannot be equated to breast feeding. Pumping and freezing breast milk and the lack of direct contact between mother and child can limit some of the positive effects of breast feeding.
Neu J: Mother’s Own Milk: Breastfeeding Medicine 2019 DOI: 10.1089/bfm.2019.0036
Possible consequences of gestational diabetes
During pregnancy, there is an elevated insulin resistance as an adaptation for the improvement of the materno-fetal nutrient transfer and to cover the nutrient requirement of the developing fetus, particularly the glucose requirements.
In about 1 of 6 pregnancies worldwide, however, there is the inability of the maternal metabolism to maintain normoglycemia, whereby the combination of insulin resistance and insufficient insulin secretion leads to gestational diabetes mellitus (GDM). The consequences of GDM on the offspring may be obesity and influences on the cardio-metabolic health. Some studies indicate that GDM has an effect on neurological and cognitive development. An improvement in the glucose and weight control in early pregnancy, or even better before conception, can reduced the risk for the offspring.
Chu AHY, Godfrey KM: Ann Nutr Metab. 2020 – DOI:10.1159/000509902
Strategies to prevent mastitis
Clinical mastitis is often a cause of discontinuing breast-feeding, therefore mastitis prevention is an important measure to promote breast-feeding.
Most of the factors that trigger mastitis can be influenced. Some of them can directly change the microbiota, like the unreasonable use of antibiotics in connection with a cesarean section delivery or recurring throat infections, unnecessary antimycotics and nipple salves or even the use of milk pumps that are not properly sterilized. Reduced plasma levels of some micronutrients such as vitamin A, zinc and antioxidants such as vitamin E and selenium are associated with subclinical mastitis. As well as mental stress and fatigue. Ultimately, certain nursing practices could be triggers.
Consultation measures
- Recommendations on the protection of the immune system of the woman and the microbiome of the milk
- Nursing advice about proper nursing practices and the right nursing technique
- Information about breast care and signs of mastitis to get professional help in a timely manner.
Flores-Quijano ME: NEST 43, Oct. November 2018 8-9
Risk factors with diabetes
Which changeable risk factors are there that are associated with unfavorable pregnancy results in women with type 1 diabetes or type 2 diabetes.
For this, the data on pregnancies in women with type 1 or type 2 diabetes were used, which were collected in the first five years of the National Pregnancy in Diabetes Audit in 170 delivery clinics in Great Britain, as well as obstetric complications (e.g. preterm birth, high birth weight, congenital anomalies, stillbirth...) for pregnancies that were concluded between January 1, 2014 and December 31, 2018. In this, connections were examined between modifiable (e.g. BMI, care before pregnancy, delivery clinic) and non-modifiable risk factors (e.g. age, ethnic origin, duration of type 1 diabetes) with pregnancy results in women with type 1 diabetes compared to those with
type 2 diabetes and connections between maternal factors and prenatal deaths. The data clarify the women with type 1 or type 2 diabetes are still confronted with unfavorable pregnancy results. The maternal blood glucose level and the BMI are the most important risk factors here that can be influenced.
Murphy HR et al.: Lancet, 2021
Videos on nutrition
Nutritional videos offer recorded lectures at international nutrition conferences and workshops with leading experts and a number of important nutrition topics. These videos and webinars are available at no cost on the website of the Nestlé Nutrition Institute and address the most discussed nutrition themes today.
The program is continually updated.
https://germany.nestlenutrition-institute.org/mediathek/videos
- Aufzeichnung des Satellitensymposium der GNPI vom 18. Juni 2021 mit Vorträgen von Mike Poßner und Jean M. Hascoët unter Vorsitz von Egbert Herting.
- Aufzeichnung des NNI Live Talk vom 30. Juni mit Vorträgen von PD Dr. Mathias Nelle, Monique Mura Knüsel und Dr. Mike Possner
- Aufzeichnung der Vorträge von: Prof. Georg Sauer, Dr. Evelyn Jantscher-Krenn, Christiane Münkwitz, Dr. Mike Poßner, Roger Ehrenreich – Stuttgart 18. Mai 2021
Info-Comics: So breast-feeding is successful
There are now two new information sheets on nursing advice from the Federal Center for Nutrition (BZfE): one for pregnant women and one for mothers after the birth. The publisher of the nursing tips is the network in cooperation with the National Breast-Feeding Committee.
The nine messages convey what breast-feeding means and how women can prepare – without giving them the feeling that it has to go perfectly. The information is clearly formulated and illustrated with colorful comic illustrations.
Gynecologists, midwives or hospital staff can use the information sheets at consultations and birth preparations courses or provide them after delivery. The information sheets as an DIN-A4 tear off pad can be ordered for free via the website www.ble-medienservice.de (order no. 0179 for pregnant women, 0180 for mothers after the birth).
Corona vaccination for pregnant women and nursing mothers
Under “Information about the coronavirus”, the Gesund ins Leben (Healthy into Life) Network provides information about the current status of vaccination against COVID-19 for pregnant women and nursing mothers and refers to the current recommendations of the obstetric associations on this:
www.gesund-ins-leben.de/fuer-familien/wissenswertes-zum-coronavirus/