Environmental and Physiological Barriers to Child Growth and Development
Summary
Aggregated analyses of child growth in low-income countries reveal a remarkably consistent picture of serious growth failure compared to the WHO reference growth curves. Birth weight is generally lower by 0.5–1.0 Z-score. Young infants then grow reasonably well until about 3 m postpartum when they enter a period of precipitate decline compared to the WHO reference to reach –2 Z-scores and worse. By 24 m this decline halts and, in many settings, there follows a period of gradual catch-up (Fig. 1). Low birthweight can be ascribed to numerous factors, especially small maternal size, which reflects the environmental effects in prior generations. Possible epigenetic mechanisms that might mediate these intergenerational effects are discussed by Silver elsewhere in this symposium.
A large proportion of the rapid growth deterioration in later infancy and the second year of life can be ascribed to infections and the wider nonspecific effects of living in an unhygienic environment. Despite never revealing themselves as clinical syndromes, the great majority of children in rural African settings are antibody positive to numerous pathogens (CMV, EB, HepB, H. pylori, and many more) by 24 m; these infections must take their toll.
Additional to these is a syndrome widely termed environmental enteric disease (EED) that combines gut leakage with a chronic inflammation leading to nutrient losses and cytokine-mediated growth retardation [1, 2].
The etiology of EED is still not entirely clear and probably results from a constellation of factors all related to poverty and pooled under the label of water, sanitation, and hygiene (WASH). Pathogens causing diarrhea play a contributory (though not necessarily dominant) role [3]. Alterations in the gut microbiota reflecting an inappropriately slow maturation toward the normal post-infancy profile [4] and/or a frank dysbiosys [5] each may play an additional role (Fig. 2).
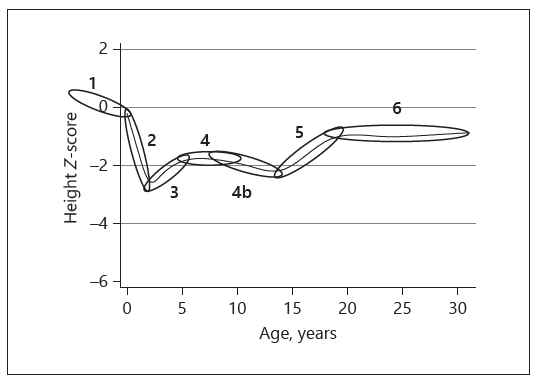
Fig. 1. Life course of stunting in rural Gambians. (1) Fetal growth retardation. (2) Precipitate decline from 3 to 24 m. (3) Spontaneous catch-up in preschoolers. (4) Stability in childhood. (4a) Artifactual decline as reference standard children enter puberty earlier. (5) Pubertal catch-up. (6) Adult status. Adapted from Prentice [6].
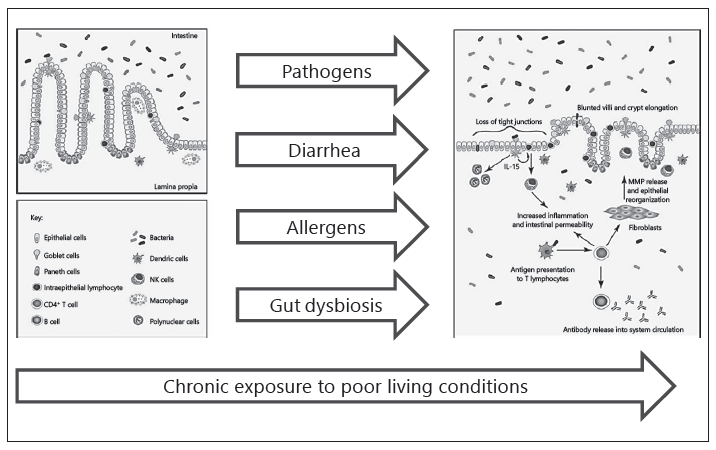
Fig. 2. Genesis and pathophysiology of environmental enteric disease (EED).
Micronutrient deficiencies, and especially iron deficiency leading to anemia, are also caused in some part by infections and inflammation that impair both their absorption and utilization.
The rapid decline in stunting and anemia rates seen in many South American countries in the past 3 or 4 decades has been well documented in Brazil where it seems clear that concerted efforts involving improved water and sanitation facilities, improvements in breast-feeding rates, poverty reduction, and mothers’ education have all contributed to the excellent progress seen. In contrast, the disappointing effects of recent WASH intervention studies (presented in this symposium by Humphrey) emphasize the need for holistic approaches that encompass a wide range of environmental improvements in addition to nutrition-specific interventions.
References
1. Harper KM, Mutasa M, Prendergast AJ, Humphrey J, Manges AR: Environmental
enteric dysfunction pathways and child stunting: s systematic review. PLoS Negl Trop
Dis 2018;12:e0006205.
2. Guerrant RL, DeBoer MD, Moore SR, Scharf RJ, Lima AA: The impoverished gut –
a triple burden of diarrhoea, stunting and chronic disease. Nat Rev Gastroenterol
Hepatol 2013;10:220–229.
3. MAL-ED Network Investigators: Relationship between growth and illness, enteropathogens and dietary intakes in the first 2 years of life: findings from the MAL-ED
birth cohort study. BMJ Glob Health 2017;2:e000370.
4. Subramanian S, Huq S, Yatsunenko T, Haque R, Mahfuz M, Alam MA, Benezra
A, DeStefano J, Meier MF, Muegge BD, Barratt MJ, VanArendonk LG, Zhang Q,
Province MA, Petri WA Jr, Ahmed T, Gordon JI: Persistent gut microbiota immaturity
in malnourished Bangladeshi children. Nature 2014;510:417–421.
5. Smith MI, Yatsunenko T, Manary MJ, Trehan I, Mkakosya R, Cheng J, Kau AL, Rich
SS, Concannon P, Mychaleckyj JC, Liu J, Houpt E, Li JV, Holmes E, Nicholson J,
Knights D, Ursell LK, Knight R, Gordon JI: Gut microbiomes of Malawian twin pairs
discordant for kwashiorkor. Science 2013;339:548–554.
6. Prentice AM, Ward KA, Goldberg GR, et al: Critical windows for interventions
against stunting. Am J Clin Nutr 2013;97;911–918.
