What Children Eat in Developing Countries: Diet in the Etiology of Undernutrition?
Abstract
We live in a world of paradoxes: one half of the world is overweight or obese with abundant access to food and the other half undernourished due to poor food access. It has been estimated that nearly 36% of children in Asia are stunted. Worldwide, approximately 1 in 4 children under the age of 5 years shows stunted growth, making the number of stunted children to 155 million; 52 million children under 5 years are wasted, of which 17 million are severely wasted. Given the wide-scale nature of global malnutrition and its long-term consequences, why has this scar in our consciousness not being addressed systematically? The Asian enigma underscores the observation that unlike other regions of the world, economic growth does not appear to keep pace with the eradication of under- nutrition. Exclusive breastfeeding is capable of maintaining adequate growth in infants in the first 3–6 months of life. Human breast milk contains the lowest protein content than any other homoeothermic animal. Despite the very low protein content of the breast milk, the protein content is sufficient for adequate infant growth. Protein deficiency is, there- fore, not the cause of undernutrition in children. Most weaning foods in developing countries are of very low energy density, high viscosity, and poor palatability. This paper suggests that it is the poor energy density of weaning food that is in part responsible for the stunting and wasting pandemic seen in developing countries. Using the concept of developing ready-to-use therapeutic food, the paper proposes an urgent need to develop high energy, low viscosity, and palatable foods. Processed foods at the village community level or on a large scale will remain one of the solutions to produce palatable and energy-dense foods. Without this intervention, our world will continue to see the ravage of malnutrition which plagues our conscience.
Diet in the Etiology of Undernutrition
We live in a world of paradoxes: one half of the world is overweight or obese with abundant access to food and the other half undernourished due to poor food access. Today, most discussions on infant nutrition focus on overweight and obesity. Whilst not diminishing the importance of this topic, the magnitude and the scale of global under nutrition in children are even stronger. This disparity starts very early in life. An examination of the infant mortality rate (IMR) in various countries illustrates this point. In many advanced countries, IMR is as low as 2–5/1,000 and in emerging countries as high as 90/1,000 (Central African Re- public) [1]: a 45-fold difference! IMR is a proxy indicator of a variety of factors that include sanitation, health, public health, and governance. A high IMR is usually associated with childhood undernutrition.
Prevalence of Stunting and Wasting
Growth is an increase in weight, height, length, and girth that occurs when humans are provided with adequate food, water, and sustenance. One of the earliest attempts to define undernutrition was described by Gomez et al. [2], who used weight for age as the classification criterion. However, this method could not distinguish between stunting and wasting. Stunting refers to a child too short for his or her age. It is the failure to grow both physically and cognitively. It results from chronic or recurrent malnutrition. The effects of stunting can last a lifetime. Wasting refers to children who are too thin for their height. Wasting or acute malnutrition is the result of recent rapid weight loss or the failure to gain weight. A child who is undernourished has an increased risk of death, morbidity, and cognitive impairment. To address these two forms of undernutrition, Waterlow [3] developed a classification method that is still widely used — even today.
It has been estimated that nearly 36% of children in South Asia and approximately 34% of children in West, Central, Southern, and Eastern Africa are stunt- ed. Similarly, the number of wasted children represents 16% in South Asia and 7–9% in Africa. In 2016, 22.9%, approximately 1 in 4 children under the age of 5 years, had stunted growth worldwide, making the number of stunted children to 155 million. In 2016, 52 million children under 5 years were wasted, of which 17 million were severely wasted globally. This translates to a prevalence of 7.7 and 2.5%, respectively [4]. Given the wide-scale nature of global malnutrition and its long-term consequences, why has this scar in our consciousness not be- ing addressed systematically? Secondly, could we provide a tangible explanation for the nature of this pandemic?
Why Is There Such a High Prevalence of Stunting and Wasting Worldwide?
In a commentary entitled the Asian Enigma, Ramalingaswami et al. [5] observed that despite rapid economic growth in Asia, childhood undernutrition still remained a major public health challenge. The Asian enigma underscores the observation that, unlike other regions of the world, economic growth does not appear to keep pace with the eradication of undernutrition.
Growth is a proxy indicator of nutritional status and well-being. A resurgence of interest in infant growth has been prompted by the observation that early growth retardation may have long-term mental and health consequences [6]. It is also an important contributor to the global burden of chronic disease. Human growth is characterized by 2 significant features. Firstly, a rapid growth velocity in the first year of life, followed by a slow growth rate until the pubertal spurt later in life (Fig. 1). Secondly, the rate of growth even in the first year of life is no more than 25–30 g/day followed by as little as 5 g/day during the subsequent years (2–9 years). This slow rate of growth continues till the child attains its pubertal spurt (Fig. 1). A closer examination of the rate of growth in the first 12 months of life demonstrates that the rate of growth is highest in the first 3 months after birth (approximately 700–900 g) per month, which then stabilizes to 500 g/month after the 6th month (Fig. 1).
Exclusive breastfeeding is capable of maintaining adequate growth in infants in the first 3–6 months of life [7–9]. Comparing the growth rate of infants in the first 3–6 months of life with the breast milk composition, we can estimate the protein and energy needs for early growth. Initial recommendations for protein and energy for normal infant growth was based on the protein and energy con- tent of human milk [9]. This can be calculated using the nutrients present in breast milk. It is known that the stage of lactation influences the nutrient contents of human milk [10]. Field studies suggest that the macronutrient composition of human milk (notably protein, fat, and carbohydrates) does not vary significantly between populations [11].
Human breast milk contains the lowest protein content compared to any other homeothermic animal [12, 13] (Table 1). This is a significant observation and further corroborates the view that the protein needs for human growth, even during the maximum growth period, is extremely small.
For over 3 decades, protein deficiency was labelled as the root cause of undernutrition in children [14]. This major focus in correcting the “protein gap” diverted attention and policies away from the real cause of undernutrition, notably an energy deficiency in infant foods [15].
Using the protein and energy content of breast milk, the amount of protein (in gram) may be converted into the percentage of protein energy by multiplying the amount of protein by the metabolizable energy conversion factor of 4 kcal or 16.7 kJ per gram of protein. This calculation is elaborated in the box below.
Protein: Energy Percent of Breast Milk
Protein content: 1.2 g/100 mL
Energy content: 70 kcal (293 kJ)/100 mL
Protein as energy = 1.2 × 4 kcal (16.7 kJ) = 4.8 kcal (20 kJ)
A mere 7% of total protein energy is all that is needed to meet the growth requirement of the infant during the first 0–6 months of life. Similarly, we can convert the protein content of any food as a percentage of total protein energy using the calculation model above.
Such a calculation on the percentage energy from protein in cereals and tubers widely used as weaning foods may be computed as illustrated in Table 2.
What is clear is that even with foods that are quantitatively low in protein, e.g ., potatoes (g/100 g), the percentage protein energy is higher than the requirements for infants (7% protein energy). This is even during the time of maximum growth (0–12 months). Lack of protein in their diet is, therefore, not the real cause of under nutrition in children living in the developing world. If the protein needs for infant growth are extremely small even at the time of maximal growth, what limits the optimal growth in these children during the weaning period? It is certainly not due to an inadequate intake of protein.
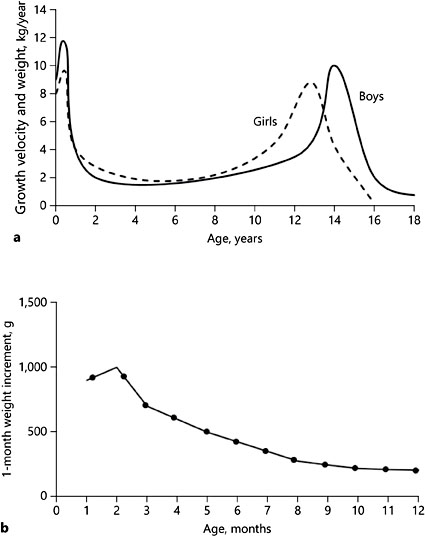
Fig. 1. Growth velocity in humans. a Growth velocity and weight. b Growth velocity in the first 12 months.
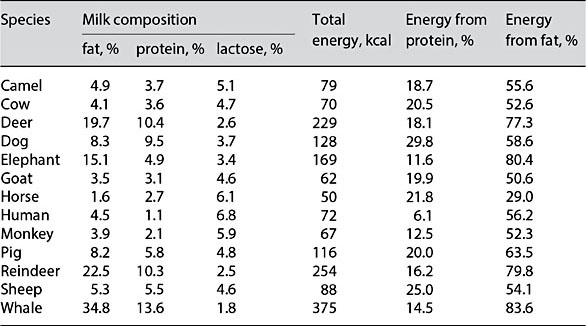
Table 1. Milk composition of humans and other animals (adapted from Jensen [12])
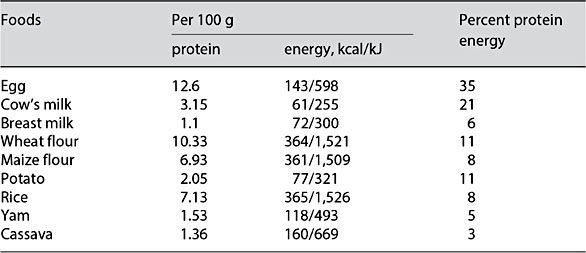
Table 2. Protein/energy of various staples compared to breast milk (using the National Nutrient Database of the United States Department of Agriculture)
Preparation of Weaning Foods in Developing Countries
The sense of taste is primordial. Apart from breast milk, weaning foods represent the second most widely exposed food during human growth. Weaning is the transition from breastfeeding to the introduction of semisolid food. It is also the most critical stage in the development of undernutrition [16].
Most weaning foods are made from carbohydrate-rich staples [17] such as ground rice, corn, cassava, yams, and plantain. These staples have to be cooked with the addition of water. During the cooking process and starch gelatinization, the carbohydrates absorb a considerable amount of water. This leads to the swelling of the starch granules with an increase in viscosity and lowering of energy density. A characteristic feature of such weaning foods is their high water content, high viscosity, and thick paste-like consistency. The preparation of weaning foods in developing countries thus poses several challenges.
An ideal weaning food must have an adequate energy density to meet the energy needs of the child. Nicol [18] was a pioneer who attempted to describe the role of energy density in defining the amount of food required to meet the energy needs of children. Subsequently, Mosha and Svanberg [17] proposed that the stomach capacity of a 1-year-old child is approximately 900–1,400 g/day. To meet the daily energy requirement of a 1-year-old child (4.2 MJ, 1,000 kcal), foods with very low energy density will need to be consumed in very large quantities. In order to meet (4.2 MJ, 1,000 kcal), the relationship between the energy density and the quantity of weaning foods to be consumed is illustrated in Figure 2. A 1-year-old child will require to consume 3–4 kg of the weaning food in order to meet their energy needs.
As an example, let us consider a mother preparing weaning food in rural India using ground rice. The weaning food needs to have an adequate mouth feel and viscosity that will enable the child to feed on this gruel safely. In order to accomplish this, she continues to add water to the gruel. As viscosity reduces and texture meets the child’s gustatory needs, the energy density of the weaning food dramatically declines (Fig. 3). A further disadvantage of preparing such carbohydrate-rich weaning food is that the “runny” texture of the weaning food at high cooking temperatures of 90°C changes into a
thick unpalatable blob upon cooling at 45° C. This is a temperature below which the weaning food is usually fed. In order to prepare the gruels with appropriate semisolid consistency, the mother continues to add further quantities of water, which results not only in producing a runny gruel but also further reduces the energy density of the gruel (Fig. 4). The reduced energy density of the weaning food, whilst making it palatable, requires impossibly large quantities of foods to be consumed. A major limitation in most weaning foods consumed in developing countries lies in its inability to meet the child’s energy needs.
In summary, if a child consumes adequate energy from weaning food, the weaning food will automatically satisfy their protein needs. Therefore, the key to optimal growth during the first 2–3 years of life is to essentially meet the child’s energy requirements.
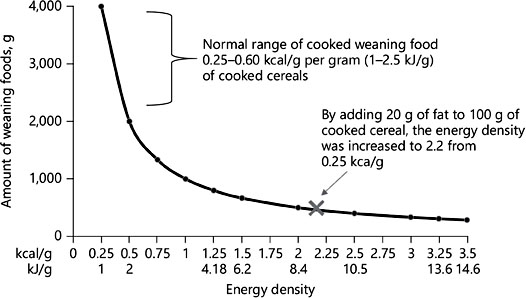
Fig. 2. Relationship between energy density (in kcal/g or kJ/g) and the amount of weaning foods to be consumed to meet 4.2 MJ/1,000 kcal
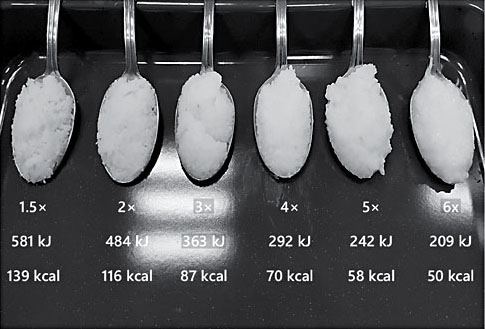
Fig. 3. Change in energy density per 100 g of gruel when diluted with various ratios of water.
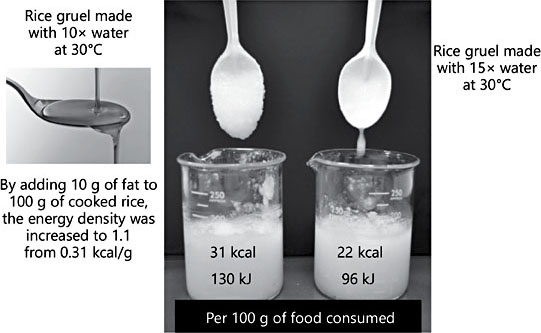
Fig. 4. Change in energy density and viscosity of cooked rice with increasing water con- tent.
Method to Improve the Energy Density of Weaning Foods
Oils and fats are the richest sources of energy per gram. The addition of fat accomplishes several advantages. Firstly, it reduces the viscosity of the gruel (making it easy for the infant to consume such starchy foods), and, most importantly, it increases palatability and energy density [19]. The addition of just 20 g of oil increases the energy density 10-fold. The relationship between the increased energy density of weaning food and the quantity of food that now needs to be consumed to meet 4.2 MJ (1,000 kcal) is shown in Figure 2. This quantity is well within the stomach capacity of infants and also appropriate to the mothers’ routine feeding pattern that may be up to 4–6 times per day.
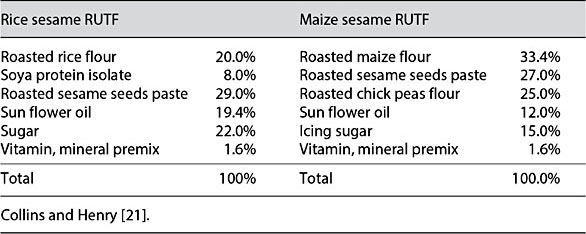
Fig. 4. Change in energy density and viscosity of cooked rice with increasing water content.
Can Ready-to-Eat Therapeutic Food Be a Model to Develop Weaning Food with High Energy Density?
Ready-to-use therapeutic food (RUTF) is a high-energy, vitamin-and mineral-fortified peanut paste mixed with dry milk products. It was first developed by Briend et al. [20] to treat severe acute malnutrition. The original recipe had 45– 60% of energy derived from fat. Historically, RUTF was developed to treat severe malnutrition. Its high energy density, long shelf life in tropical conditions, and the facility to consume it without cooking made it a valuable therapeutic food in the treatment of severe undernutrition.
In an attempt to develop RUTF based on locally available cereal and oil seeds, Collins and Henry [21] produced a range of products based on rice, corn, wheat, along with soya and sesame seed (Table 3). An additional reason for developing such products was to exclude the use of peanuts that are potentially allergenic and are easily contaminated with aflatoxin. Locally developed RUTF has now been produced and expanded in the treatment of malnutrition [22]. Learning from the experience of developing locally made RUTF: can this concept be used to develop high-energy weaning foods? The induction of undernutrition in developing countries can be partly attributed to the consumption of low-energy-dense weaning foods. It is abundantly clear that undernutrition is not due to the lack of protein in the diet but the lack of energy-dense foods.
The following question arises: can we develop an appropriate weaning food based on the RUTF concept? This is a challenge that the present paper poses. Such a project will only be possible if there is close collaboration with private- public partnerships. At the present time, there is a raging debate on the consumption of ultra processed food and its implication in the etiology in diabetes, obesity, and other chronic diseases [23]. It is instructive to point out that in the case of producing appropriate weaning foods for use in the developing world, processed food will remain one of the solutions to produce a palatable and energy-dense food.
Several challenges still remain in the development of local weaning foods. This includes the type of fat to be used particularly in relation to brain development. Most of the oils used in preparing energy-dense weaning foods are high in ω-6 linoleic acid but poor in essential fatty acids. They are also very low in ω-3 α-linolenic acid [24].
Conclusion
There is an urgent need for the development of low-cost weaning foods that have adequate energy and micronutrient content. Much remains to be investigated in the application of simple technology and alternative methods to reduce the high viscosity and improve the energy density of weaning foods. It is increasingly evident that the provision of weaning foods with sufficient energy still remains a challenge in many developing countries. This imbalance in meeting the energy needs of a child appears to be one of the major contributors in generating the vast number of stunted and wasted children globally.
Given that stunted children have a compromised brain development and cognition, the future challenge is to focus on providing nutritionally adequate weaning foods to realize the full potential of these children. This paper has identified the need to provide weaning foods with adequate energy and nutrients to optimize growth and development. In many developing countries, even today, it is not the lack of protein but the lack of energy in the diet that leads to wasting and stunting. An understanding of the nature and ethology of undernutrition is necessary before any strategy can be evolved. Stunting and wasting still remains a pervasive pandemic in most of Asia, Africa, and Latin America. Using the model of RUTF, it is proposed that further focus and attention is provided in developing a low-cost, high-energy, nutrient-rich weaning food. Without this intervention, our world will continue to see the ravages of malnutrition which plagues our conscience.
References
-
1 UN Inter-Agency Group for Child Mortality Estimation. Mortality Rate, Infant (per 1,000 Live Births) 2017. http://www.childmortality. org/.
-
2 Gomez F, Ramos G, Frenk S, et al: Mortality in second and third degree malnutrition. J Trop Pediatr (Lond) 1956;2:77–83.
-
3 Waterlow JC: Classification and definition of protein-calorie malnutrition. Br Med J 1972; 3:566–569.
-
4 Lu C, Black MM, Richter LM: Risk of poor development in young children in low-in- come and middle-income countries: an estimation and analysis at the global, regional, and country level. Lancet Glob Health 2016; 4:e916–e922.
-
5 Ramalingaswami V, Jonsson U, Rohde J: The Asian enigma; in: The Progress of Nations. New York, UNICEF, 1996.
-
6 Widdowson E, McCance R: A review: new thoughts on growth. Pediatr Res 1975;9:154.
-
7 Food and Agriculture Organization/World Health Organization: Energy and Protein Requirements. Report of a Joint FAO/WHO Ad Hoc Expert Committee. WHO Technical Re- port Series 522. Geneva, WHO, 1973.
-
8 Butte NF, Garza C, Smith EB, Nichols BL: Human milk intake and growth in exclusively breast-fed infants. J Pediatr 1984;104:187– 195.
-
9 World Health Organization: Energy and Protein Requirements: Report of a Joint FAO/ WHO/UNU Expert Consultation. Geneva, WHO, 1985.
-
10 Lönnerdal B: Effects of maternal dietary intake on human milk composition. J Nutr 1986;116:499–513.
-
11 Garza C, Johnson CA, Smith E, Nichols BL: Changes in the nutrient composition of human milk during gradual weaning. Am J Clin Nutr 1983;37:61–65.
-
12 Jensen R: Handbook of Milk Composition. San Diego, Academic Press, 1995.
-
13 Heinig MJ, Nommsen LA, Peerson JM, et al: Energy and protein intakes of breast-fed and formula-fed infants during the first year of life and their association with growth velocity: the DARLING Study. Am J Clin Nutr 1993;58:152–161.
-
14 Mclaren D: The great protein fiasco. Lancet 1974;304:93–96.
-
15 Waterlow J, Payne P: The protein gap. Nature 1975;258:113–117.
-
16 Black RE, Allen LH, Bhutta ZA, et al: Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 2008;371:243–260.
-
17 Mosha AC, Svanberg U: The acceptance and intake of bulk-reduced weaning foods: the Luganga village study. Food Nutr Bull 1990; 12:69–74.
-
18 Nichol BM: Protein and calorie concentration. Nutr Rev 1971;29:83–88.
-
19 Walker AF, Pavitt F: Energy density of Third World weaning foods. Nutr Bull 1989;14:88– 101.
-
20 Briend A, Lacsala R, Prudhon C, et al: Ready- to-use therapeutic food for treatment of marasmus.Lancet 1999;353:1767–1768.
-
21 Collins S, Henry J: Alternative RUTF formulations. Community-based therapeutic care (CTC). Emerg Nutr Network Suppl 2004;2: 35–37.
-
22 Choudhury N, Ahmed T, Hossain MI, et al: Ready-to-use therapeutic food made from locally available food ingredients is well accepted by children having severe acute malnutrition in Bangladesh. Food Nutr Bull 2018;39:116–126.
-
23 Monteiro CA, Moubarac JC, Cannon G, et al: Ultra‐processed products are becoming dominant in the global food system. Obes Rev 2013;14(suppl 2):21–28.
-
24 Brenna JT, Akomo P, Bahwere P, et al: Balancing omega-6 and omega-3 fatty acids in ready-to-use therapeutic foods (RUTF). BMC Med 2015;13:117.