Vitamin D in Toddlers
Key Messages
- Young children are at risk of low vitamin D intakes and status
- National surveys, prospective cohorts, and dietary intervention studies have shown that fortification of foods consumed by toddlers is a safe and effective approach to increasing their vitamin D intakes and status
- Dose-response trials in 1 to 3-year-olds are still needed to estimate the actual vitamin D requirement among toddlers
Background
Young children and toddlers (1–3 years) are at risk of nutrient deficiencies due to their limited appetite relative to their high requirements for growth and development. Vitamin D has been identified as a risk nutrient for toddlers in many countries. Vitamin D is a fat-soluble vitamin that is obtained from a combination of skin synthesis during sunshine exposure and from the diet. As it has a key role in the regulation of calcium and phosphorus metabolism, vitamin D is critical for healthy bone growth and development in childhood. Prevention of very low vitamin D status is also important for robust immune function.
Vitamin D in the Diets of Young Children
Due to the extended winter period, people resident at high latitudes need to obtain sufficient vitamin D from the diet for prevention of vitamin D deficiency. Foods containing substantial amounts of naturally occurring vitamin D are limited and not consumed on a regular basis by young children. Small but important amounts of vitamin D3 are found in commonly consumed staple foods, such as meat, dairy, and eggs. Vitamin D2 (ergocalciferol) can be obtained from irradiated mushrooms. Depending on regional legislation, some foods are fortified with vitamin D, including milk, infant formula, yogurt, spread, cheese, juice, bread, and breakfast cereals. In addition, vitamin D is available as a dietary supplement, either as vitamin D2 or vitamin D3.
Recommended Intakes of Vitamin D in Toddlers
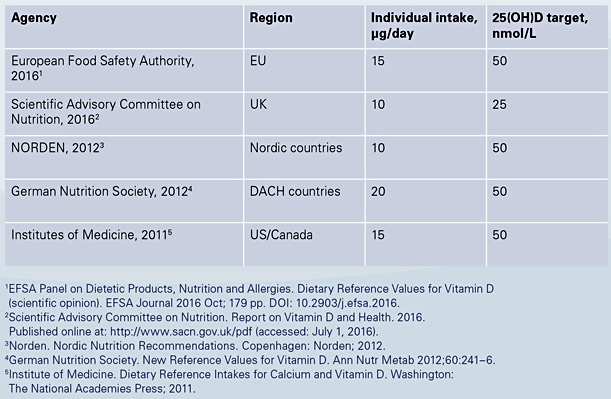
Current recommendations for individual intakes of vitamin D in Europe and North America vary between countries, from 10 to 20 µg/day (400 to 800 IU), shown in Table 1. Based on adult recommendations, these are the intakes of vitamin D that will achieve circulating 25-hydroxyvitamin D (25(OH)D) concentrations (the bio-marker of vitamin D status) of 25–50 nmol/L, for the prevention of adverse bone health outcomes.
Intakes of Vitamin D among Toddlers Relative to Recommendations
Vitamin D intakes among young children are generally between 2 and 9 µg/ day, including countries with mandatory or voluntary vitamin D fortification [1]. While nutritional supplements can be important contributors to vitamin D intake, current rates of supplement use among toddlers are often low [2, 3]. Key food sources of vitamin D in toddlers are vitamin D-fortified milks, formula, breakfast cereals and yogurts, meat, and eggs [4]. Even in countries where voluntary fortification with vitamin D is widespread, almost all children have intakes of vitamin D below 10 µg/day [3].
Is There Evidence for Low Vitamin D Status among Toddlers?
Evidence for extensive low vitamin D status is mixed, and it seems that average 25(OH)D concentrations among children decrease with increasing age, possibly due to reducing milk intake. In the UK National Diet and Nutrition Survey among 1.5- to 3-year-olds, the prevalence of year-round plasma 25(OH)D concentrations <25 nmol/L was 8% [5]. In a study of 741 toddlers from the prospective Cork BASELINE Birth Cohort, the year-round prevalence of serum 25(OH)D <25 nmol/L was 1.6%, and 4.6% were <30 nmol/L, which increased to 8.6% during the winter months (November to April) [1]. In this cohort, over a quarter of the children had a 25(OH)D concentration <50 nmol, which reached almost half the study cohort in winter. Apart from season, consumption of at least 5 µg/day of vitamin D and consumption of fortified infant formula were the main determinants of circulating 25(OH)D. In Montreal in 2013, El Hayek et al. [6] reported that despite 95% of 508 preschoolers having vitamin D intakes <10 µg/day, plasma 25(OH)D was >50 nmol/L in 88% of them, which was likely due to the dual effect of fortified milk provision and skin synthesis.
Ways to Improve Intakes/Status of Vitamin D
The current dietary supply of vitamin D is not sufficient to close the large gap between dietary intakes and recommendations for vitamin D in toddlers, and many children are at risk of low vitamin D status during this growing period. While vitamin D-containing supplements can increase vitamin D intakes and status, this is only true for supplement users. From a public health policy perspective, food fortification with vitamin D is likely to be the best option for increasing vitamin D intakes and status across the population distribution. Milk and milk products are widely consumed among toddlers, and there is abundant evidence from large observational studies [1–4, 6, 7], trials [8], and a recent systematic review of trials [9] that consumption of vitamin D-fortified milk or formula increases vitamin D intake and status, without the risk of excessive intakes or adverse effects.
In summary, dose-response randomized controlled trials in children aged 1–3 years are still required to estimate the vitamin D requirement of young children and to make evidence-based recommendations. From a public health nutrition perspective, fortified foods provide a feasible solution to ensuring an adequate dietary supply of vitamin D in toddlers.
References
- Ní Chaoimh C, McCarthy EK, Hourihane JO’BH, Kenny LC, Irvine AD, Murray DM, et al. Low vitamin D defi ciency in Irish toddlers despite northerly latitude and a high prevalence of inadequate intakes. Eur J Nutr. 2018 Mar;57(2):783–94.
- Bailey RL, Catellier DJ, Jun S, Dwyer JT, Jacquier EF, Anater AS, et al. Total usual nutrient intakes of US children (under 48 months): fi ndings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr. 2018 Sep;148(9S):1557S–1566S.
- Hennessy A, Browne F, Kiely M, Walton J, Flynn A. The role of fortified foods and nutritional supplements in increasing vitamin D intake in Irish preschool children. Eur J Nutr. 2017 Apr;56(3):1219–31.
- Moyersoen I, Lachat C, Cuypers K, Ridder K, Devleesschauwer B, Tafforeau J, et al. Do current fortification and supplementation programs assure adequate intake of fat-soluble vitamins in Belgian infants, toddlers, pregnant women, and lactating women? Nutrients. 2018 Feb;10(2):E223.
- Bates B, Lennox A, Prentice A, Bates C, Page P, Nicholson S, Swan G. National Diet and Nutrition Survey. Results from Years 1–4 (combined) of the Rolling Programme (2008/2009–2011/2012). London: Public Health England; 2014.
- El Hayek J, Pham TT, Finch S, Hazell TJ, Jean-Philippe S, Vanstone CA, et al. Vitamin D status in Montreal preschoolers is satisfactory despite low vitamin D intake. J Nutr. 2013 Feb;143(2):154–60.
- Maguire JL, Lebovic G, Kandasamy S, Khovratovich M, Mamdani M, Birken CS, et al. The relationship between cow’s milk and stores of vitamin D and iron in early childhood. Pediatrics. 2013 Jan;131(1):e144–51.
- Akkermans MD, Eussen SR, van der Horst-Graat JM, van Elburg RM, van Goudoever JB, Brus F. A micronutrient-fortified young-child formula improves the iron and vitamin D status of healthy young European children: a randomized, double-blind controlled trial. Am J Clin Nutr. 2017 Feb;105(2):391–9.
- Brett NR, Gharibeh N, Weiler HA. Effect of vitamin D supplementation, food fortifi cation, or bolus injection on vitamin D status in children aged 2-18 years: a meta-analysis. Adv Nutr. 2018 Jul;9(4):454–64.
