Malnutrition
Treatment of underfed infants < 6 months
Severe acute malnutrition is increasingly being observed in infants under 6 months of age and is often associated with a higher mortality rate in infants than in older infants and children.
Apart from causal factors such as low birth weight, persistent diarrhoea and chronic underlying diseases or a disability, the development of severe acute mal- nutrition in infants under 6 months of age is caused by inadequate nutrition, especially due to inadequate breastfeeding practices.
There are essential physiological differences between toddlers and older children, which require modified management approaches or clinical interventions. The WHO has developed a number of recommendations for the identification and treatment of severe acute malnutrition in infants under the age of 6 months.
The most important WHO recommendations:
Infants < 6 months of age with severe acute malnutrition should receive the same general medical care as infants > 6 months of age with severe acute malnutrition.
Priority should be given to introducing or restoring an effective exclusive nursing period by the mother or other caregiver.
Infants under the age of 6 months can be discharged from care if they are breastfeeding effectively or feeding well with replacement feeds, have gained sufficient weight and have a weight-for-length 2 ≥-z-score according to the WHO Child Growth Standards median.
Infant malnutrition in Germany
As part of the current children’s health report by the Techniker Krankenkasse, the
occurrence of malnutrition in the analysis group was examined as well – with some surprising results.
The TK Children’s Health Report follows the TK’s Birth Report from 2017 with the caption “A routine data analysis on Caesarean section and preterm birth”. It examined the connection between maternal illnesses and diseases of the child related to the
factors of Caesarean section and premature birth. Childhood overweight and obesity are health risks that can have long-term consequences. However, forms of malnutrition must also be taken into consideration– and treated.
Malnutrition is more common among children than obesity in the TK analysis group. The term does not refer to being underweight, but primarily dehydration and a lackof vitamin D, proteins and minerals.
Malnutrition is determined in almost 5 per cent of newborns. The value rises to around 7 per cent at the age of 1 year, drops to almost 5 per cent in the 2nd year of life, and to around 2 per cent in the following years. The prevalence in the analysis group
was 18.7 per cent over the course of the entire investigation period.
A connection is demonstrated in preterm infants with a 30.5 per cent increased risk of malnutrition. This applies to girls and boys in equal measure.
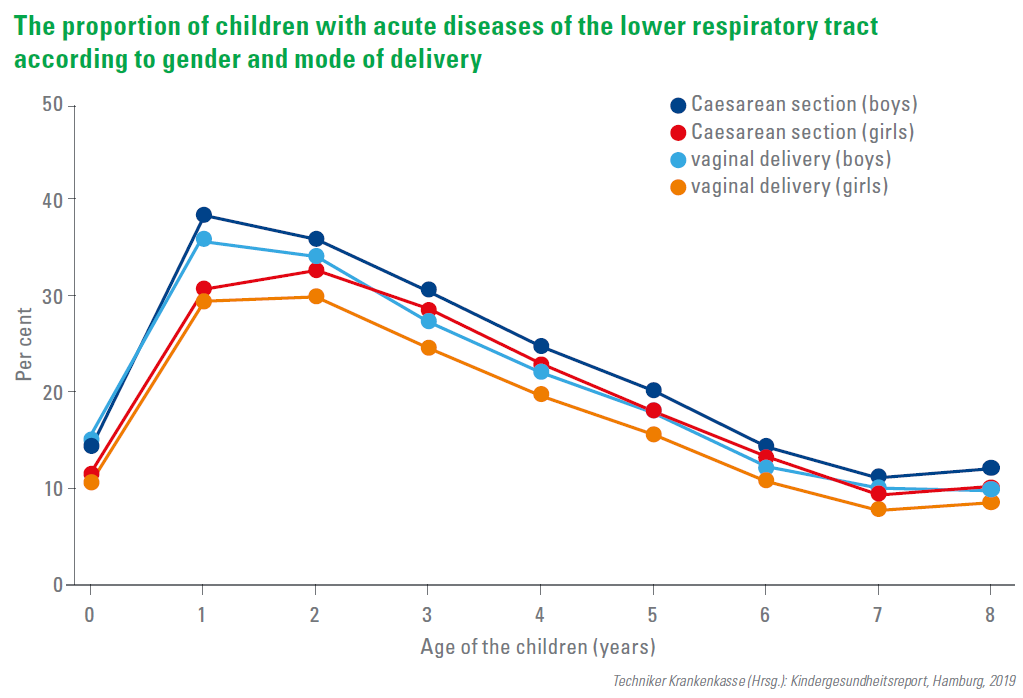
This applies to girls and boys in equal measure. However, a link with a Caesarean section can be demonstrated with a 7 per cent higher probability in the first eight years of life.
A similar picture as that of malnutrition is also evident in the “symptoms of food intake” disease cluster. This concerns nutritional problems and improper nutrition, abnormal weight gain or loss.
The overall prevalence is 21.3 per cent. In infants, the proportion was around 7 per cent, also with the peak at 1 year (around 10%). Again, preterm infants (28.2%) and C-section infants (10.9%) are particularly affected by this. Boys have a significantly higher risk (12.9%) than girls (8.9%).
Vitamin D deficiency: There is a lack of awareness
In the year 2012, the D-A-CH Nutrition Societies quadrupled their vitamin D intake
recommendations per day, thus underlining the significance of these vitamins. The question, though, is whether the new recommendations for an increased vitamin D intake improve the widespread state of vitamin D deficiency in German children and adolescents.
Vitamin D is a key component in the growth and the development of children and adolescents and affects a number of functions. Epidemiological and clinical studies across the world have shown that at least 25(OH)D blood values of ≥ 20.0 ng/
ml (≥ 50.0 nmol/L), which have been defined as sufficient vitamin D values by several but not all international and national nutrition and children’s organisations, are often not achieved.
For a study spanning 6 years (January 2009 to December 2014) in Mülheim an der Ruhr, healthy children and adolescents (n=1,929, 1–17 years, median 11.0 years, 46.9% female) consulting a paediatric group practice were recruited. 75 per cent of the study participants were German or European (Caucasian) origin. The remaining had mostly Turkish roots, 2% showed a worldwide distribution.
The median 25(OH)D serum concentrations between 2009–2012 and 2013–2014 after increasing recommendations for vitamin D intake from 200 IU (5 μg) to 800 IU (20 μg), did not show a significant difference. The D-A-CH recommendations had no influence on vitamin D levels in children and adolescents. The prevalence of vitamin D deficiency has not changed compared to previous studies.
Guidelines should be drawn up to ultimately improve the health of the population. This requires the general population to be aware of the significance and implication of vitamin D deficiency. Efforts must be made to ensure at least the agreed minimum of around 1000 IU/day for healthy bones in young children and adolescents.
