Iron Nutriture of the Fetus, Neonate, Infant, and Child
Key Messages
- Iron requirements are high in neonates and infants, particularly in premature babies.
- Breast milk is low in iron, and breastfed infants should be offered additional sources of iron.
- Iron deficiency is the most common micronutrient deficiency in children and causes deficits in exercise capacity and neurodevelopment.
Abstract
Iron is a key nutrient and is essential for the developing fetus, neonate, infant, and child. Iron requirements are high during early stages of life because it is critically important for the production of new red blood cells and muscle cells as well as brain development. Neonates, infants, and children obtain iron from dietary sources including breast milk (lactoferrin) and heme- and non-heme-containing foods. Iron deficiency (ID) is the most common micronutrient deficiency in children and pregnant women worldwide. ID and iron deficiency anemia (IDA) can affect growth and energy levels as well as motor and cognitive performance in the developing child.
The fetus is completely dependent on maternal iron crossing through the placenta and, although it is generally well protected against deficiency at birth, ID in mothers can increase the risk of ID and IDA in their children as early as 4 months. This review will discuss the uses of iron, iron requirements, and the sources of iron from conception through childhood. In addition, it will describe the prevalence and clinical manifestations of ID and IDA in children and discuss recommendations for iron supplementation of children and pregnant women.
Introduction
Iron is an essential nutrient during all stages of human development. It has particular importance for children because of its critical impact on their development. In the human body, iron is found mainly in (1) hemoglobin in red blood cells (RBCs) and erythroblasts; (2) myoglobin in muscle cells and in other iron-containing proteins such as cytochromes and, catalases (15%); (3) transferrin-bound iron in circulation; (4) storage proteins such as ferritin and hemosiderin. It is essential for DNA replication and many other metabolic processes. By far the biggest use of iron is in the production of new RBCs. However, in infants and children, muscle growth and production of new myoglobin are also important consumers of iron.
Table 1. Definitions of anemia
| Population | Hemoglobin, g/dL |
| Pregnant women | 11 |
| Infants | 11 |
| Children aged 6 months to <5 years | 11 |
| Children aged 5 to <12 years | 11.5 |
| Children aged 12 to <15 years | 12 |
Iron status is regulated by intestinal absorption and transport, and there is no controlled mechanism for iron excretion. In adults, dietary iron sources provide only 5% of the daily needs and the remainder is obtained by recycling iron released during the breakdown of old RBCs. In contrast, infants and children must obtain 30% of their daily iron from their diet to provide the necessary iron for new muscle cells and RBCs [1] .
Iron deficiency (ID) is the most common micronutrient deficiency in children [2, 3] . Anemia, primarily caused by ID, disproportionally impacts young children and pregnant mothers.
In the US, 7–9% of children ages 1–3 years have ID. However, the worldwide burden is much higher with an estimated 43% globally in 2011 and approximately 70% in Central and West Africa [4] . As will be discussed in more detail below, ID during fetal development and the first 2 years of life is associated with poor growth and decreases in cognitive, motor, and social emotional development [5–7] . Both the United States Department of Health and Human Services and the World Health Organization (WHO) have set goals to reduce ID and iron deficiency anemia (IDA). The WHO priorities have now been adopted as Priority Nutrition Indicators for the United Nation’s post-2015 Sustainable Development Goals [8, 9] .
Definitions of ID in Early Life
Iron is categorized as a Type 1 nutrient. During ID, as in all Type 1 nutrient deficiencies, a child will continue to grow, but tissue depletion of the nutrient occurs and causes specific clinical symptoms [10] . Routine screening for ID and IDA between 6–24 months is recommended, especially for children living in areas with a high prevalence of ID. The minimum laboratory screen for IDA is hemoglobin and the guidelines outlined in Table 1 can be used to define anemia. In upper-income countries, a full blood count is obtained, which will give hemoglobin, hematocrit, mean corpuscular volume, and RBC distribution width. In children with IDA, mean corpuscular volume will be decreased and RBC distribution width will most likely be increased. In some settings, ferritin is also measured as part of the screening process. However, ferritin values can be misleading in children living in areas where the infectious disease burden is high because ferritin is also an acute-phase protein.
Effects of ID on Neurodevelopment
The strongest evidence for an effect on neurological outcomes comes from studies done on cognition in school-aged children and teenagers with ID and IDA
[11]. A recent meta-analysis in older children and adults showed evidence of a modest improvement in the cognitive domains of concentration, intelligence, memory, psychomotor skills, and scholastic achievement after iron supplementation [12] . The effects of ID and iron supplementation in young children are less clear. Further details are summarized by Pasricha and colleagues [13] in an accompanying paper in this issue.
Children and infants with ID also have decreased psychomotor and mental development, but the timing, degree, and duration of the deficiency may all have profound effects on how and when these symptoms manifest. The brain is not a homogenous organ and different regions of the brain develop more rapidly at different times in development [14] . For example, in the last trimester of pregnancy there is rapid myelination and development of the striatum and the hippocampus. In children between the ages of 6 months and 3 years there is also rapid myelination and the frontal cortex and basal ganglia (motor control) are both developing most rapidly [15] . Infants with ID can have multiple symptoms that are consistent with impaired hippocampal function, reduced myelination, and altered temperament and altered dopamine metabolism. For example, iron-deficient infants can present with decreased attention and memory [16, 17] ; deficits in visual and auditory systems [18, 19]; and altered temperament and social and emotional behaviors [20–22] . Taken together, the evidence implies that ID in early life can permanently alter the brain and nervous system and may explain at least in part why little efficacy has been shown on neurodevelopmental outcomes in iron supplementation trials in young children [23–26] .
Effects of ID on Immunity and Susceptibility to Infection
Iron has opposing effects on immunity and susceptibility to infection. It can decrease efficacy of and cytokine production by lymphocytes [27, 28] , and recent work has shown that it has detrimental effects on the phagocytic activity or macrophages and oxidative burst in neutrophils [29] . On the other hand, ID can be protective against certain infectious diseases including malaria in both children [30–32] and pregnant women [33, 34] . Further information on this is described by Prentice [35] in this issue.
Effects of ID on Exercise Capacity
Iron is an essential element for the transportation of oxygen and is a cofactor for enzymes involved in aerobic metabolism. ID and IDA both impair exercise capacity and increase fatigue [36, 37] .
Iron during Fetal Development
Iron is critical for rapidly developing and proliferating cells. During fetal development, iron plays a profound role in organ development, particularly the brain. Evidence suggests that iron is of particular importance to the hippocampus which is rapidly developing during the late stages of gestation [38] . Of course, the region of the brain affected by in utero ID (and therefore subsequent clinical effects observed in the infant) depends on the magnitude of the deficiency and when in pregnancy the deficiency begins. In addition, it is essential for the fetus to acquire adequate iron stores from its mother to sustain growth during the first 6 months of life when the iron intake from breast milk is very low (see below).
The fetus obtains iron from the mother through the placenta and 80% is transferred during the third trimester of pregnancy [39] . Transferrin-bound iron is transferred directly from the maternal blood to the syncytiotropho-blast in the placental villi via transferrin receptor 1 (TFR1). After binding to iron (Fe3+) on the apical side of the syn-cytiotrophoblast, holotransferrin with its bound iron is internalized and the iron is released into the cytoplasm. The trophoblasts may also take up non-transferrin-bound iron via ZIP8 or ZIP14 [40, 41] and heme iron via LRP1 [42]. No matter which pathway it uses to enter the cell, all non-heme iron is released from the basal side of syncytiotrophoblast via ferroportin (FPN). It remains unclear how iron is transported across the fetal endothelium and then to fetal transferrin [43] , and pathways for heme iron are still not fully described.
The regulation of iron transport from the mother to the fetus across the placenta is thought to be controlled by the fetus for the following reasons: (1) infants of anemic women are usually born with normal iron status [44] and (2) fetal signals of iron status and gestational age can influence expression of TFR1 on the placenta [43] . One molecule which may influence placental iron transport is fetal hepcidin [45] , but the role of maternal hepcidin remains unclear [46] . Recent evidence indicates that the placenta upregulates iron (and zinc) transporters in response to maternal deficiency [47] .
The prevalence of ID is high during pregnancy, and 43% of pregnant women worldwide are anemic. ID accounts for 50–75% of anemia cases and is thought to be largely due to inadequate diet and increased nutritional requirements during pregnancy [48] . However, inflammation also plays a role by downregulating absorption (see Prentice [35] in this issue). It is general policy for pregnant mothers worldwide to be routinely supplemented with iron [49] . The US Center for Disease Control recommends that all pregnant women take a 30 mg/day iron supplement [50] and the WHO recommends supplementation with 30–60 mg/day [51] . However, the UK takes a very different view. Based on evidence that iron absorption is physiologically upregulated in pregnancy and that cessation of menstruation also reduces iron losses, there is no increase in the recommended nutrient intake for iron and supplements are only recommended if there is evidence of anemia [52] . The clinical benefits of maternal iron supplementation on birth outcomes (including preterm delivery, low birth weight, and neonatal morbidity and mortality) are still unclear despite decades of research [49] . A systematic review in 2015 found that routine iron supplementation reduced maternal IDA at birth (relative risk 0.29, 95% CI 0.17–0.49) but did not have consistent benefits on pregnancy outcome [53] . Part of the problem may be that iron is rarely compared against a true placebo control. Notably, a recent trial from Kenya using true controls reported a robust effect on birth weight with a large benefit in women who were iron deficient [54] . In addition, there is no definitive evidence showing that iron supplementation of nonanemic women improves maternal or infant outcomes. An alternate strategy recommended by the WHO to improve the infant’s body stores of iron is delayed cord clamping after birth [55, 56] . The timing of delayed clamping varies between studies but is generally done between 1 and 5 min after delivery, or at the end of umbilical cord pulsations [57]. This can impart an estimated 80 mL of blood transfer after 1 min and 100 mL by 3 min which will impart an extra 40–500 mg/kg of iron and has been shown to have a significant benefit on ferritin levels in the infant at 6 months [58] .
Iron during the Neonatal Period and Early Childhood
At birth most full-term infants have high to normal hemoglobin concentrations (15–17 g/dL) and then remain iron replete until 6 months of life. As noted above, babies of mothers with ID and IDA are at increased risk of ID, but this deficiency develops at 4–6 months and is not apparent at birth. Premature babies have overall greater nutritional needs and higher iron requirements than healthy full-term babies ( Table 2 ) [59] . Premature infants often also have lower iron stores than full-term infants and are at increased risk of developing ID and IDA [60] .
There are 3 main dietary sources of iron: breast milk (where iron is bound to lactoferrin), heme iron, and non-heme iron. For neonates and very young infants, the only sources of iron are breast milk and/or formula. The concentration of iron in breast milk is very low and declines over time from 0.6 mg/L at 2 weeks to 0.3 mg/L at 5 months postpartum [62] . (Note that for a 4-kg baby who is likely to consume around 800 mL breast milk its intake would be about one-fifth of the value recommended in Table 2 ; but see comments below about the high bioavail-ability.) Current evidence suggests that if a mother has severe anemia, breast milk concentration decreases further, but not if a mother has mild-moderate anemia [63].
The iron in breast milk is highly bioavailable (50% compared to 3–4% in infant formula), although the precise mechanisms of absorption remain unclear [64] . The iron in breast milk is found in iron-binding proteins, predominantly lactoferrin. Lactoferrin is one of the most abundant proteins in milk [64] . It is a single polypeptide chain (MW 75–90K) that can bind 2 molecules of ferric iron [65] and closely resembles transferrin (the iron-carrying protein in serum) [66] . Like transferrin, lactoferrin functions as both an iron carrier molecule and an iron chelator. For example, transferrin in normal human circulation is only 30–40% saturated with iron, which makes over half of its binding sites available to bind excess iron and accounts for its bacteriostatic activity [67] . The extent to which lactoferrin is saturated with iron in breast milk is uncertain (one estimate suggests 10%); however, it is known to possess bacteriostatic properties which are at least in part attributable to its unsaturated iron-binding capabilities [68] . Lactoferrin is most likely absorbed in the small intestine of infants and neonates [69] .
Table 2. Daily iron requirements during childhood [61]
| Age | Recommended dietary amount |
| Full-term | 1 mg/kg |
| Premature | 2-4 mg/kg |
| 1- to 3-year-olds | 7 mg |
| 4- to 8-year-olds | 10 mg |
| 9- to 13-year-olds | 8 mg |
| 14- to 18-year-old boys | 11 mg |
| 14- to 18-year-old girls | 15 mg |
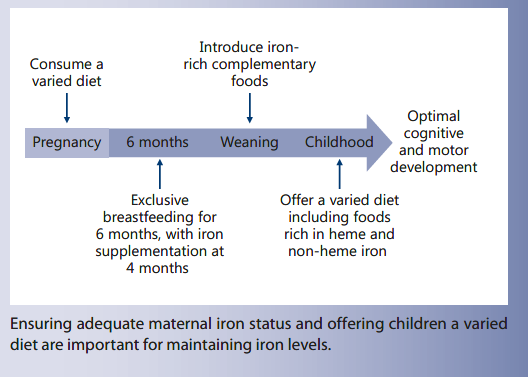
As will be discussed in more detail below, while iron supplementation can correct anemia at any stage, there is little evidence to support the idea that iron supplementation can correct neurodevelopmental deficits caused by iron deprivation in utero or in early childhood. Hence, current evidence suggests that it is important to provide a source of iron for children during the first 2 years of life [7, 70, 71] . Both the WHO [72] and the American Academy of Pediatrics [73] recommend exclusive breastfeeding for 6 months. It is recommended that full-term breastfed infants should start an iron supplement at 4 months (elemental iron 1 mg/kg daily, maximum 15 mg) and the supplement should be continued until the infant is taking sufficient quantities of iron-rich complementary foods [1]. If formula is used, full-term infants should be given iron-fortified formulas [74] . Human milk is also the recommended food for preterm babies, but human milk alone does not supply adequate amounts of iron, protein, calcium, phosphorous, and other micronutrients [75] . Hence, human milk fortifiers, iron supplements, and/or specially formulated preterm formula are often recommended [74] . Breastfed premature infants should start an iron supplement at 2 weeks of age and continue until 1 year of age [59, 71].
Full-term and preterm babies should be taking complementary foods by 6 months of age [76, 77] . Iron-rich complementary foods include meat (lamb, chicken, beef, and pork), baby cereals (including fortified rice), and some vegetables (green beans, peas, and spinach) [76, 78] .
Iron during Childhood
Iron is obtained entirely from dietary sources; hence, it is important that children are offered a diverse diet with a variety of iron-rich foods in order to provide an adequate intake of iron ( Table 2 ). Children who do not eat at least 3 servings of iron-rich foods/day may benefit from an iron supplement [1]. Heme iron is the most bioavailable form of iron and is readily absorbed from meat, poultry, and fish. Non-heme iron is available from vegetables (especially spinach, lentils, and pumpkin seeds) and fortified cereals. Fortified cereals are the major source of iron for most children in the United States [79] . Other important sources of non-heme iron include beans (kidney, lima, and navy beans) and nuts. Absorption of non-heme iron is increased by foods rich in vitamin C (oranges, grapefruit, broccoli, tomatoes) and decreased by phytate (in bran, oats, and rye fiber), polyphenols (in tea, coffee, and cocoa), dietary calcium, and soy proteins. Calcium inhibits the absorption of iron by as much as 60% and thus there is a risk of ID in children who drink more than 700 mL of cow’s milk per day [50].
Conclusions
Iron requirements are high during all stages of human development. ID and IDA result in deficits in growth, neurological development, exercise capacity, and immune function. The recommended dietary allowances (RDA) are 1 mg/kg for full-term infants, 2–4 mg/kg for premature infants, 7 mg for 1- to 3-year-olds, 10 mg for 4- to 8-year-olds, and 9–13 mg for 9- to 13-year-olds. Iron sources include lactoferrin in breast milk as well as heme and non-heme iron from other dietary sources. Iron supplementation should be implemented if a child has a low hemoglobin level, does not have access to 3–4 servings per day of iron-rich foods, or lives in an area with a high prevalence of ID.
It is important that children are offered a diverse diet with a variety of iron-rich foods in order to provide an adequate intake of iron
Disclosure Statement
The author declares that no financial or other conflict of interest exists in relation to the contents of the paper. The writing of this article was supported by Nestlé Nutrition Institute.
Funding Sources
The author is supported by MCA760-5QX00 to the MRC International Nutrition Group by the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement.
References
- Mahoney DH: Iron deficiency in infants and young children: screening, prevention, clinical manifestations, and diagnosis; in Motil KJ, Drutz JE, Hoppin AG (eds): UpToDate.
- Global Burden of Disease Pediatrics Collaboration, Kyu HH, Pinho C, Wagner JA, Brown JC, Bertozzi-Villa A, et al: Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the Global Burden of Disease 2013 Study. JAMA Pediatr 2016; 170: 267–287.
- Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al: A systematic analysis of global anemia burden from 1990 to 2010. Blood 2014; 123: 615–624
- Engle-Stone R, Aaron GJ, Huang J, Wirth JP, Namaste SM, Williams AM, et al: Predictors of anemia in preschool children: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr 2017; 106: 402S–415S.
- Lozoff B: Iron deficiency and child development. Food Nutr Bull 2007; 28:S560–S571.
- Clark KM, Li M, Zhu B, Liang F, Shao J, Zhang Y, et al: Breastfeeding, mixed, or formula feeding at 9 months of age and the prevalence of iron deficiency and iron deficiency anemia in two cohorts of infants in China. J Pediatr 2017; 181: 56–61.
- Geng F, Mai X, Zhan J, Xu L, Zhao Z, Georgieff M, et al: Impact of fetal-neonatal iron deficiency on recognition memory at 2 months of age. J Pediatr 2015; 167: 1226–1232.
- Bates-Eamer N, Carin B, Lee M, Lim W, Kapila M: Post-2015 Development Agenda: Goals, Targets And Indicators – Special Report. 2015.
- United Nations Standing Committee on Nutrition: Nutrition and the Post-2015 Sustainable Development Goals. A Technical Note. October 2014.
- Golden MH: Specific deficiencies versus growth failure: type I and type II nutrients. SCN News 1995; 10–14.
- Low M, Farrell A, Biggs B-A, Pasricha S-R: Effects of daily iron supplementation in pri-mary-school-aged children: systematic review and meta-analysis of randomized controlled trials. CMAJ 2013; 185:E791–E802.
- Falkingham M, Abdelhamid A, Curtis P, Fairweather-Tait S, Dye L, Hooper L: The effects of oral iron supplementation on cognition in older children and adults: a systematic review and meta-analysis. Nutr J 2010; 9: 4.
- Larson LM, Phiri KS, Pasricha S-R: Iron and cognitive development: what is the evidence. Ann Nutr Metab 2017;71(suppl 3):25–38.
14 Wachs TD, Georgieff M, Cusick S, McEwen BS: Issues in the timing of integrated early interventions: contributions from nutrition, neuroscience, and psychological research. Ann NY Acad Sci 2014; 1308: 89–106. - Wachs TD, Georgieff M, Cusick S, McEwen BS: Issues in the timing of integrated early interventions: contributions from nutrition, neuroscience, and psychological research. Ann NY Acad Sci 2014; 1308: 89–106.
- Cusick SE, Georgieff MK: The role of nutrition in brain development: the golden opportunity of the “first 1000 days.” J Pediatr 2016; 175: 16–21.
- Burden MJ, Westerlund AJ, Armony-Sivan R, Nelson CA, Jacobson SW, Lozoff B, et al: An event-related potential study of attention and recognition memory in infants with iron-deficiency anemia. Pediatrics 2007; 120:e336–e345.
- Geng F, Mai X, Zhan J, Xu L, Zhao Z, Georgieff M, et al: Impact of fetal-neonatal iron deficiency on recognition memory at 2 months of age. J Pediatr 2015; 167: 1226–1232.
- Algarin C, Karunakaran KD, Reyes S, Morales C, Lozoff B, Peirano P, et al: Differences on brain connectivity in adulthood are present in subjects with iron deficiency anemia in infancy. Front Aging Neurosci 2017; 9: 54.
- Roncagliolo M, Garrido M, Walter T, Peira-no P, Lozoff B: Evidence of altered central nervous system development in infants with iron deficiency anemia at 6 mo: delayed maturation of auditory brainstem responses. Am J Clin Nutr 1998; 68: 683–690.
- Wachs TD, Pollitt E, Cueto S, Jacoby E, Creed-Kanashiro H: Relation of neonatal iron status to individual variability in neonatal temperament. Dev Psychobiol 2005; 46: 141–153.
- Lozoff B, Clark KM, Jing Y, Armony-Sivan R, Angelilli ML, Jacobson SW: Dose-response relationships between iron deficiency with or without anemia and infant social-emotional behavior. J Pediatr 2008; 152: 696– 702, 702.31–33.
- Algarín C, Nelson CA, Peirano P, Wester-lund A, Reyes S, Lozoff B: Iron-deficiency anemia in infancy and poorer cognitive inhibitory control at age 10 years. Dev Med Child Neurol 2013; 55: 453–458.
- Steinmacher J, Pohlandt F, Bode H, Sander S, Kron M, Franz AR: Randomized trial of early versus late enteral iron supplementation in infants with a birth weight of less than 1,301 g: neurocognitive development at 5.3 years’ corrected age. Pediatrics 2007; 120: 538–546.
- Wang B, Zhan S, Gong T, Lee L: Iron therapy for improving psychomotor development and cognitive function in children under the age of three with iron deficiency anaemia. Cochrane Database Syst Rev 2013; 6: CD001444.
- Pasricha S-R, Hayes E, Kalumba K, Biggs B-A: Effect of daily iron supplementation on health in children aged 4–23 months: a systematic review and meta-analysis of ran-domised controlled trials. Lancet Glob Health 2013; 1:e77–e86.
- Lukowski AF, Koss M, Burden MJ, Jonides J, Nelson CA, Kaciroti N, et al: Iron deficiency in infancy and neurocognitive functioning at 19 years: evidence of long-term deficits in executive function and recognition memory. Nutr Neurosci 2010; 13: 54–70.
- Thibault H, Galan P, Selz F, Preziosi P, Olivier C, Badoual J, et al: The immune response in iron-deficient young children: effect of iron supplementation on cell-mediated immunity. Eur J Pediatr 1993; 152: 120–124.
- Galan P, Thibault H, Preziosi P, Hercberg S: Interleukin 2 production in iron-deficient children. Biol Trace Elem Res 1992; 32: 421– 426.
- Hassan TH, Badr MA, Karam NA, Zkaria M, El Saadany HF, Abdel Rahman DM, et al: Impact of iron deficiency anemia on the function of the immune system in children. Medicine (Baltimore) 2016; 95:e5395.
- Gwamaka M, Kurtis JD, Sorensen BE, Holte S, Morrison R, Mutabingwa TK, et al: Iron deficiency protects against severe Plasmodi-um falciparum malaria and death in young children. Clin Infect Dis 2012; 54: 1137–1144.
- Jonker FAM, Calis JCJ, van Hensbroek MB, Phiri K, Geskus RB, Brabin BJ, et al: Iron status predicts malaria risk in Malawian preschool children. PLoS One 2012; 7:e42670.
- Nyakeriga AM, Troye-Blomberg M, Dorf-man JR, Alexander ND, Bäck R, Kortok M, et al: Iron deficiency and malaria among children living on the coast of Kenya. J Infect Dis 2004; 190: 439–447.
- Kabyemela ER, Fried M, Kurtis JD, Mutabingwa TK, Duffy PE: Decreased susceptibility to Plasmodium falciparum infection in pregnant women with iron deficiency. J Infect Dis 2008; 198: 163–166.
- Senga EL, Harper G, Koshy G, Kazembe PN, Brabin BJ: Reduced risk for placental malaria in iron deficient women. Malar J 2011; 10: 47.
- Prentice AM: Clinical implications of new insights into hepcidin-mediated regulation of iron absorption and metabolism. Ann Nutr Metab 2017;71(suppl 3):40–48.
- Rowland TW, Kelleher JF: Iron deficiency in athletes. Insights from high school swimmers. Am J Dis Child 1960 1989; 143: 197– 200.
- Rowland TW, Deisroth MB, Green GM, Kelleher JF: The effect of iron therapy on the exercise capacity of nonanemic iron-deficient adolescent runners. Am J Dis Child 1960 1988; 142: 165–169.
- Krebs NF, Lozoff B, Georgieff MK: Neurodevelopment: the impact of nutrition and inflammation during infancy in low-resource settings. Pediatrics 2017; 139:S50–S58.
- Widdowson EM, Spray CM: Chemical development in utero. Arch Dis Child 1951; 26: 205–214.
- Wang C-Y, Jenkitkasemwong S, Duarte S, Sparkman BK, Shawki A, Mackenzie B, et al: ZIP8 is an iron and zinc transporter whose cell-surface expression is up-regulated by cellular iron loading. J Biol Chem 2012; 287: 34032–34043.
- Hojyo S, Fukada T, Shimoda S, Ohashi W, Bin B-H, Koseki H, et al: The zinc transporter SLC39A14/ZIP14 controls G-protein coupled receptor-mediated signaling required for systemic growth. PLoS One 2011; 6: e18059.
- Cao C, Pressman EK, Cooper EM, Guillet R, Westerman M, O’Brien KO: Placental heme receptor LRP1 correlates with the heme exporter FLVCR1 and neonatal iron status. Reproduction 2014; 148: 295–302.
- Cao C, Fleming MD: The placenta: the forgotten essential organ of iron transport. Nutr Rev 2016; 74: 421–431.
- Allen LH: Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr 2000; 71: 1280S–1284S.
- Young MF, Griffin I, Pressman E, McIntyre AW, Cooper E, McNanley T, et al: Maternal hepcidin is associated with placental transfer of iron derived from dietary heme and non-heme sources. J Nutr 2012; 142: 33–39.
- Koenig MD, Tussing-Humphreys L, Day J, Cadwell B, Nemeth E: Hepcidin and iron homeostasis during pregnancy. Nutrients 2014; 6: 3062–3083.
- Jobarteh ML, McArdle HJ, Holtrop G, Sise EA, Prentice AM, Moore SE: mRNA levels of placental iron and zinc transporter genes are upregulated in Gambian women with low iron and zinc status. J Nutr 2017; 147: 1401– 1409.
- Di Renzo GC, Spano F, Giardina I, Brillo E, Clerici G, Roura LC: Iron deficiency anemia in pregnancy. Womens Health (Lond) 2015; 11: 891–900.
- Mwangi MN, Prentice AM, Verhoef H: Safety and benefits of antenatal oral iron supplementation in low-income countries: a review. Br J Haematol 2017; 177: 884–895.
- Recommendations to prevent and control iron deficiency in the United States. Centers for Disease Control and Prevention. MMWR Recomm Rep 1998; 47: 1–29.
- WHO: WHO recommendations on antenatal care for a positive pregnancy experience. Available from: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/ (accessed February 10, 2017).
- Dietary reference values for food energy and nutrients for the United Kingdom. Report of the Panel on Dietary Reference Values of the Committee on Medical Aspects of Food Policy. Rep Health Soc Subj (Lond) 1991; 41: 1– 210.
- Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al: Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health 2013; 1:e16–e25.
- Mwangi MN, Roth JM, Smit MR, Trijsburg L, Mwangi AM, Demir AY, et al: Effect of Daily antenatal iron supplementation on Plasmodium infection in Kenyan women: a randomized clinical trial. JAMA 2015; 314: 1009–1020.
- Andersson O, Domellöf M, Andersson D, Hellström-Westas L: Effects of delayed cord clamping on neurodevelopment and infection at four months of age: a randomised trial. Acta Paediatr 1992 2013; 102: 525–531.
- World Health Organization: Guideline: Delayed Umbilical Cord Clamping for Improved Maternal and Infant Health and Nutrition Outcomes. Geneva, World Health Organization, 2014. Available from: http:// www.ncbi.nlm.nih.gov/books/NBK310511/ (accessed August 28, 2017).
- Bayer K: Delayed umbilical cord clamping in the 21st century: indications for practice. Adv Neonatal Care 2016; 16: 68–73.
- Committee on Obstetric Practice, American College of Obstetricians and Gynecologists: Committee Opinion No.543: Timing of umbilical cord clamping after birth. Obstet Gynecol 2012; 120: 1522–1526.
- Martin CR, Ling P-R, Blackburn GL: Review of infant feeding: key features of breast milk and infant formula. Nutrients 2016; 8: 279.
- Mills RJ, Davies MW: Enteral iron supplementation in preterm and low birth weight infants. Cochrane Database Syst Rev 2012; CD005095.
- Institute of Medicine; Food and Nutrition Board: Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc: A Report of the Panel on Micronutrients. Washington, DC, National Academies Press, 2001.
- Siimes MA, Vuori E, Kuitunen P: Breast milk iron – a declining concentration during the course of lactation. Acta Paediatr Scand 1979; 68: 29–31.
- Kumar A, Rai AK, Basu S, Dash D, Singh JS: Cord blood and breast milk iron status in maternal anemia. Pediatrics 2008; 121:e673– e677.
- Andreas NJ, Kampmann B, Mehring Le-Do-are K: Human breast milk: a review on its composition and bioactivity. Early Hum Dev 2015; 91: 629–635.
- Ward PP, Uribe-Luna S, Conneely OM: Lac-toferrin and host defense. Biochem Cell Biol Biochim Biol Cell 2002; 80: 95–102.
- Wally J, Buchanan SK: A structural comparison of human serum transferrin and human lactoferrin. Biometals 2007; 20: 249–262.
- Lin L, Pantapalangkoor P, Tan B, Bruhn KW, Ho T, Nielsen T, et al: Transferrin iron starvation therapy for lethal bacterial and fungal infections. J Infect Dis 2014; 201: 254–264.
- Jiang R, Lopez V, Kelleher SL, Lönnerdal B: Apo- and holo-lactoferrin are both internalized by lactoferrin receptor via clathrin-mediated endocytosis but differentially affect ERK-signaling and cell proliferation in Caco-2 cells. J Cell Physiol 2011; 226: 3022– 3031.
- Lönnerdal B, Bryant A: Absorption of iron from recombinant human lactoferrin in young US women. Am J Clin Nutr 2006; 83: 305–309.
- Berglund SK, Westrup B, Hägglöf B, Hernell O, Domellöf M: Effects of iron supplementation of LBW infants on cognition and behavior at 3 years. Pediatrics 2013; 131: 47–55.
- MacQueen BC, Baer VL, Scott DM, Ling CY, O’Brien EA, Boyer C, et al: Iron supplements for infants at risk for iron deficiency. Glob Pediatr Health 2017; 4: 2333794X17703836.
- McGuire S: World Health Organization. Comprehensive Implementation Plan on Maternal, Infant, and Young Child Nutrition. Geneva, Switzerland, 2014. Adv Nutr 2015; 6: 134–135.
- Breastfeeding and the use of human milk. American Academy of Pediatrics, Work Group on Breastfeeding. Breastfeed Rev 1998; 6: 31–36.
- Schanler RJ: Nutritional composition of human milk and preterm formula for the premature infant; in Abrams SA, Hoppin AG (eds): UpToDate, 2016.
- Schanler RJ, Garza C: Plasma amino acid differences in very low birth weight infants fed either human milk or whey-dominant cow milk formula. Pediatr Res 1987; 21: 301–305.
- Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, et al: Complementary feeding: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2008; 46: 99–110.
- Gupta S, Agarwal R, Aggarwal KC, Chellani H, Duggal A, Arya S, et al: Complementary feeding at 4 versus 6 months of age for pre-term infants born at less than 34 weeks of gestation: a randomised, open-label, multi-centre trial. Lancet Glob Health 2017; 5:e501– e511.
- Walter T, Dallman PR, Pizarro F, Velozo L, Peña G, Bartholmey SJ, et al: Effectiveness of iron-fortified infant cereal in prevention of iron deficiency anemia. Pediatrics 1993; 91: 976–982.
- Subar AF, Krebs-Smith SM, Cook A, Kahle LL: Dietary sources of nutrients among US children, 1989–1991. Pediatrics 1998; 102: 913–923.
Reprinted with permission from: Cerami Ann Nutr Metab 2017;71(suppl 3):8–14 DOI: 10.1159/000481447