Human Milk Oligosaccharides versus Prebiotics Oligosaccharides
Human Milk Oligosaccharides versus Prebiotic Oligosaccharides
Clemens Kunz
Key Messages
- Both human milk oligosaccharides (HMOs) and prebiotic oligosaccha-rides (PBOs) belong to the large class of carbohydrates, but they have completely different structures
- HMOs and PBOs have a high potential for various functions
- However, to date, there has been no human study showing similar or comparable functions
Background
The concept of prebiotics has received much attention during the last decade. Prebiotic oligosaccharides (PBOs) are discussed to have various health benefits mainly due to an influence on the colonic microbial composition or activity [1–3].
During the last 5 years, research on human milk oligosaccharides (HMOs) has developed into one of the “hottest” topics in infant nutrition, especially due to the enormous progress in producing some of these components on a large scale (Fig. 1). Today, some HMOs can be added to infant formula or used for other purposes. Therefore, we are at the beginning of a new era in infant nutrition [4].
In the following, a few basic questions will be addressed.
What Are “Prebiotics”?
The first definition was published in 1995 by Gibson and Roberfroid [5]: “Prebiotics are nondigestible food ingredients that beneficially affect the host by selectively stimulating the growth and/or activity of one or a limited number of bacteria in the colon that
can improve host health.” Although this definition has been modified over the years, it has not been possible to phrase a more specific description [2]. This, however, would help to clearly describe “a prebiotic effect in infants.” A most recent consensus statement states that a prebiotic is “a substrate that is selectively utilized by host microorganisms conferring a health benefit” [3].
What Does a “Prebiotic Effect in Infants” Mean?
In studies involving human infants, there are different opinions about what a “prebiotic effect” is. Often, studies concentrate on various goals:
- Determination of the total number of Bifidobacteria is reported; however, today we know that not all Bifidobacteria can utilize HMOs or gala-tooligosaccharides (GOS)/fructooligosaccharides (FOS). It is important to investigate not only Bifidobacteria subspecies but also the interaction between the different microorganisms in infants.
- If no effect on the microbiota can be found, authors will focus on the production of short-chain fatty acids such as butyrate, acetate, or propionate, and others.
- If no effect can be found on such metabolites either, investigators will concentrate on the effect on fecal consistency to compare, e.g., the effects of galactosylated oligosaccha-rides with those of breast-feeding.
As there is no clear definition of what is meant by “a prebiotic effect has been found,” the question “how can it be concluded that GOS, FOS, and other PBOs have the same prebiotic effect as HMOs” arises. 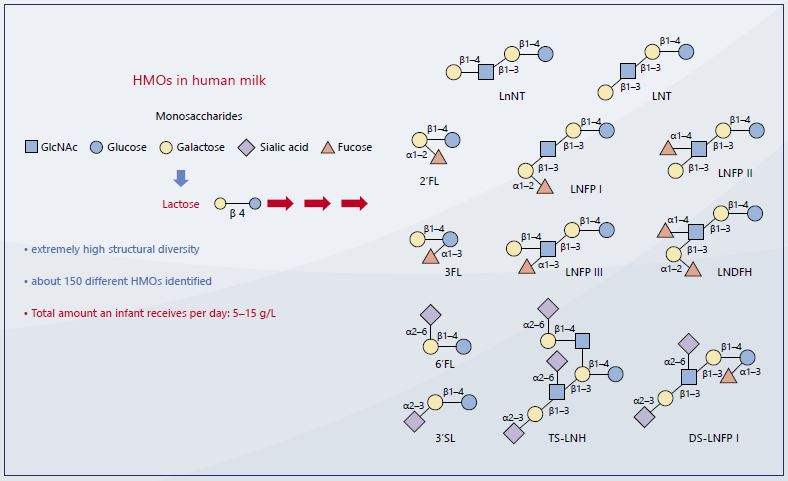
Figure 1: Examples of the complexity of single HMOs with a high potential for specifc functions due to their different linkages between monosaccharides. No other biological fluid contains such a high variety and structures as human milk [6].
Is There a Similarity between PBOs and HMOs?
In most scientific publications, PBOs are compared and considered to be similar to or even identical with HMOs, including reviews on their functional aspects. Some infant formula-producing companies go as far as to claim in consumer information that both groups of carbohydrates share similarities regarding structure and function.
However, although PBOs and HMOs belong to the same chemical class of carbohydrates, they do not share structural similarities that would be necessary to speculate about similar biological functions. If there were structural similarities, human studies would be needed to definitely show (i) what a “prebiotic effect” specifically means and (ii) that PBOs such as GOS and FOS show the same effects as HMOs in infants?
To demonstrate the difference between GOS/FOS and HMOs, two major aspects have to be considered: (i) the monosaccharide composition and
(ii) the linkage between them. The latter is of particular importance, since specific functions including defence mechanisms, immune functions, or anti-inflammatory effects strongly depend on those linkages.
In prebiotics added to infant formula, the main monosaccharides are, e.g., galactose, glucose, fructose, xy-lose, and arabinose. Except for glucose and galactose, these monosaccharides are not present in human milk (Fig. 2). In HMOs, specific monosaccharides are N-acetyl-glucosamine, fucose, and N-acetyl-neuraminic acid (sialic acid), which cannot be found in PBOs.
Where Do HMOs Come from?
Naturally, HMOs are solely produced in the lactating mammary glands. Only recently it has become possible to produce some of them on a large scale by various means. To differentiate between HMOs from the mammary gland and technically produced HMOs, I suggest to called the latter “identical HMOs” (iHMOs), since they are the same as those produced in lactating mothers.
Are GOSs and FOSs Present in Human Milk?
GOS and FOS are not present in human milk. For commercial reasons, some companies conclude that the addition of GOS and FOS to infant formula will bring them closer to human milk. However, there is no structural similarity between PBOs and HMOs. This is even the case for “galactosylated oligosaccharides from milk” (a term that can be found on the label of commercial products). Those GOS from milk are synthesized by lactose, either cleaving off glucose and galactose or using lactose itself, to elongate it by the attachment of galactose moieties in various numbers. These linear short or longer GOS still share no structural similarity with HMOs either. So far, no study has been carried out proving that the effects of GOS/FOS on, e.g., the immune system are comparable to those of HMOs.
What Is Needed?
In recent years, major advances have been made in the field of prebiotics, mainly influenced by the progress made in understanding the role of the micro-biota in health and disease. Effective strategies to achieve a healthy micro-biota are certainly needed. In this context, the appropriate use of the term “prebiotics” would be helpful, but this also requires a more specific definition.
Figure 2: Monosaccharide composition of human milk oligosaccharides (HMOs) and prebiotics (PBOs) (a) and examples of specific linkages (b) 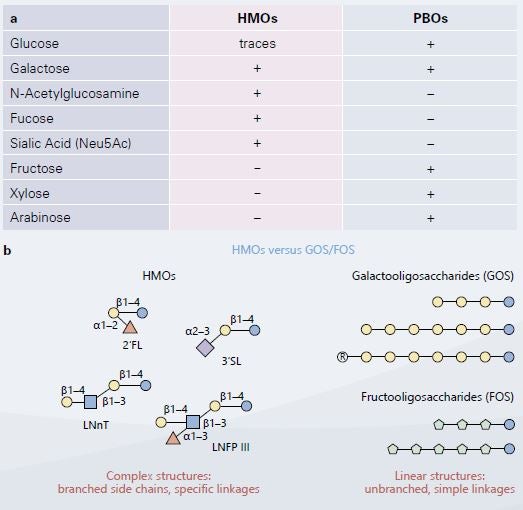
References
- Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014 Aug;11(8):506–14.
- Hutkins RW, Krumbeck JA, Bindels LB, Cani PD, Fahey G Jr, Goh YJ, et al. Prebiotics: why definitions matter. Curr Opi Biotechnol. 2016 Feb;37:1–7.
- Gibson GR, Hutkins R, Sanders ME, Prescott SL, Reimer RA, Salminen SJ, et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol. 2017 Aug;14(8):491–502.
- Kunz C, Kuntz S, Rudloff S. Bioactivity of human milk oligosaccharides. In Moreno FJ, Sanz ML (eds). Food Oligosaccharides: Production, Analysis, and Bioactivity. Chichester; John Wiley & Sons, Inc. 2014. p 5–17. ISBN: 978–1–118–42649–4.
- Gibson GR, Roberfroid MB. Dietary modulation of the human colonic microbiota: introducing the concept of prebiotics. J Nutr. 1995 Jun;125(6):1401–12.
- Morozov V, Hansmann G, Hanisch FG, Schroten H, Kunz C. Human milk oligosaccharides as promising antivirals. Mol Nutr Food Res. 2018 Mar;62(6): e1700679.
