The Human Milk Microbiome – An Important New Twist in Infant Nutrition
The Human Milk Microbiome – An Important New Twist in Infant Nutrition
Michelle McGuire
Key Messages
- Human milk microbiomes vary across women, geographies, and cultures
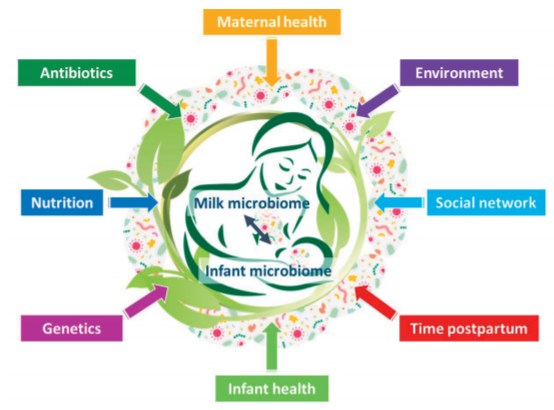
- Factors such as maternal diet, maternal health, and use of antibiotics might have important effects on milk microbiome variation
- The origin of breastmilk's microbiome and its potential impact on maternal and infant health still require much more research
Experts have historically assumed that human milk was sterile unless produced by a woman with mastitis or contaminated. However, with the emergence of high-tech methods whereby scientists can now identify bacteria via their genetic profiles rather than having to grow them in the laboratory, researchers now agree that human milk contains a unique and rich variety of not only bacteria but also viruses and fungi.
Interestingly, the most abundant bacteria present in the human milk microbiome, even when produced by healthy women, are not what one might expect, they are Staphylococcus and Streptococcus. Furthermore, and in line with the microbiomes of other biological niches like the vagina and skin, every woman appears to have her own signature milk microbiome – seemingly a reflection of her own lifelong experiences and exposures –, and typical milk microbiomes vary across geographies and cultures. Scientists know almost nothing about what factors drive this variation, but mounting evidence suggests that maternal diet, maternal health (for instance, obesity), and antibiotic use might be important. In addition, fascinating work stemming from small-scale hunter-gatherers and farmers living in the Central African Republic suggest that seasonality, an infant’s social life, and variation in childcare patterns among mother-infant dyads might also help to shape both the diversity and composition of the bacteria that find their way into breastmilk.
There are several hypotheses as to the origin of breastmilk bacteria. One is that bacteria in the mother’s intestines are selectively taken up by immune cells and trafficked to the breasts. This possibility is supported by studies showing that when lactating mothers consume probiotic supplements, the bacteria in the supplements show up both in the milk they produce and their infants’ feces. Controlled animal studies also support a direct link between a mother’s gut bacteria and the bacteria found in her milk. In addition, it is possible that bacteriapresent in the infant’s mouth help colonize the breast (and, thus, become incorporated into the milk) during suckling. This possibility is supported by findings that the bacterial communities found in a breastfed infant’s mouth are very similar to those found in human milk. Indeed, ultrasound images have shown that the contents of an infant’s mouth move back into the breast with each suckle. Testing these hypotheses, which might actually both be true, will require additional controlled human intervention studies. In addition, the question as to how variation in these bacteria impact maternal and infant health has not been answered.