Globesity and Increasing Noncommunicable Diseases
Globesity, the global obesity epidemic, has become a significant concern affecting individuals across various age groups from infancy to the elderly. Adult obesity is more prevalent worldwide than undernutrition, while pediatric obesity rates have reached approximately 5.9% in children under 5 years. The impact of obesity extends to both communicable and noncommunicable diseases. Notably, during the COVID-19 pandemic, obesity was associated with worse outcomes, including increased disease severity and mortality [1]. Furthermore, the lockdown measures implemented during the pandemic resulted in reduced physical activity, contributing to a significant increase in BMI among children aged 2–19 years as reported by Kompaniyets and colleagues [1].
Obesity is strongly linked to noncommunicable diseases, leading to substantial medical and economic burdens. It affects multiple organ systems, resulting in various comorbidities such as idiopathic intracranial hypertension, systemic hypertension, metabolic-associated liver disease, gall bladder disease, pulmonary function abnormalities, obstructive sleep apnea, increased cancer risk, and endocrine abnormalities, among others.
The etiology of obesity is complex and involves both unmodifiable and modifiable factors. Unmodifiable factors include genetics, ethnicity, and intrauterine factors, while modifiable factors encompass diet, lifestyle, socioeconomic status, physical activity, sleep patterns, and dysbiosis [2].
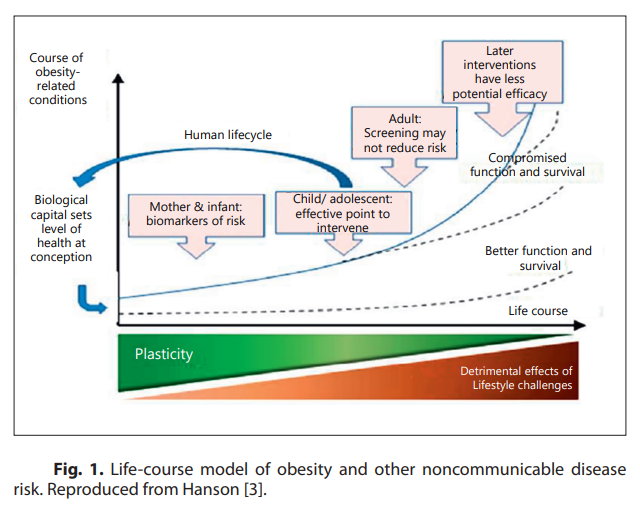
Efforts should be directed toward preventing and managing the globesity epidemic through a comprehensive, multimodal integrated action plan that addresses different levels of prevention. The primary goal of this action plan is to achieve and maintain an energy balance throughout an individual's lifespan. Early intervention is crucial due to increased plasticity and reduced adverse effects of lifestyle changes, aligning with the life course model of obesity and noncommunicable diseases (Fig. 1) [4].
Intervening early to break the cycle of childhood obesity is fundamental. This can be achieved by reducing obesity in pregnant women, promoting breastfeeding as the optimal postnatal nutrition, and ensuring proper formula preparation for infants who are not breastfed. It is well-established that high protein content in infant formula during the first year of life can have insulinogenic and adipogenic effects. Therefore, using lower protein infant formula can positively impact BMI trajectories up to 11 years, resulting in similar BMI values at adiposity rebound as observed in breastfed infants [5].
Supplementing infant formula with human milk oligosaccharides is essential to maintain a healthy intestinal microbiota. Preserving microbiota homeostasis and preventing dysbiosis have implications for preventing obesity, metabolic syndrome, and noncommunicable diseases [6].
In addition, healthy weaning practices and promoting a balanced diet for toddlers and children are crucial. This includes limiting the consumption of sugary and fatty foods and beverages and curtailing their promotion on television and digital media. Implementing clear labeling for food products containing high sugar, high fat, trans fat, saturated fat, and artificial sweeteners should be mandatory. Further measures, such as banning the sale of unhealthy foods in schools and increasing taxes on such products, can help reduce their consumption [4].
Promoting physical activity and encouraging children and their parents to engage in regular exercise are important strategies. Additionally, maintaining adequate sleep duration is beneficial in supporting overall health and well-being. It is crucial to monitor healthy nutrition practices throughout the human life cycle, with the active involvement of pediatricians and society as a whole, for the effective prevention and management of obesity [4].
References
1 Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death – United States, MarchDecember 2020. MMWR Morb Mortal Wkly Rep. 2021;70(10):355–61.
2 Lifshitz F, Lifshitz JZ. Globesity: the root causes of the obesity epidemic in the USA and now worldwide. Pediatr Endocrinol Rev. 2014;12(1):17–34.
3 Hanson M. Nurturing human capital along the life course: investing in early childhood development. Presented at World Health Organization, Geneva, 10–11 January 2013. Available from: https://www.who.int/publications/i/item/9789241505901
4 Bhisma M. Childhood stunting, wasting, and obesity, as critical global health issues: forging cross-sectoral solutions. 7th International Conference on Public Health; 2022. Available from: http://theicph.com/en_US/concepts-principles-andpolicy-approaches-to-tackling-health-inequity/
5 Totzauer M, Escribano J, Closa-Monasterolo R, Luque V, Verduci E, ReDionigi A, et al. Different protein intake in the first year and its effects on adiposity rebound and obesity throughout childhood: 11 years follow-up of a randomized controlled trial. Pediatr Obes. 2022;17(12):e12961.
6 West CE, Renz H, Jenmalm MC, Kozyrskyj AL, Allen KJ, Vuillermin P, et al. The gut microbiota and inflammatory noncommunicable diseases: associations and potentials for gut microbiota therapies. J Allergy Clin Immunol. 2015;135(1):3–13.
