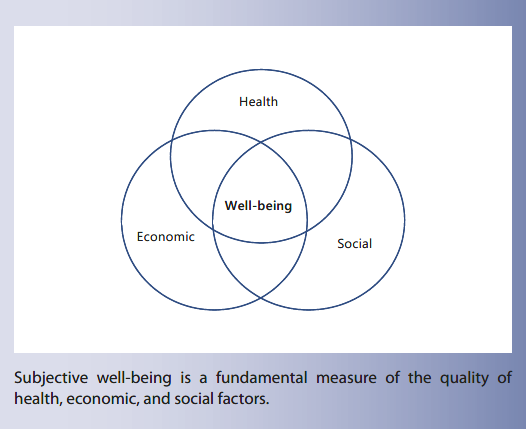
Determinants of Well-Being and Their Implications for Health Care
Key Messages
-
Having an umbrella measure of subjective well-being permits the relative importance of its sources to be compared, making it possible to move beyond a general wish to improve well-being to establishing a standard for comparison of alternative policies, both within and beyond health care.
-
Subjective well-being research results underscore the importance of the social context as a first-order determinant of health and happiness.
-
Some have argued that it is misleading to use “happiness” as a generic term to cover subjective well-being more generally. While “subjective well-being” is more precise, it simply does not have the convening power of “happiness.”
-
The World Happiness Report uses 6 variables, including national averages for Gross Domestic Product per capita, World Health Organization measures of healthy life expectancy, and 4 more socially oriented variables, to explain roughly three- quarters of the variation across countries and over time in annual national average life evaluations from usually 1,000 respondents to the Gallup World Poll in each of more than 150 countries.
-
It has been calculated that to raise 6 key variables from the world’s lowest levels to their world averages would raise a nation’s average life evaluations by almost 2 points on the 0–10 scale, with almost 1.2 points due to having more people with someone to count on in times of trouble. This social support effect alone is more than the estimated impact of the 18-fold increase in GDP per capita required to shift the poorest country to the world average.
Keywords
Happiness · Subjective well-being · Social prescribing · Reforming health care · Wellness · Sources of happiness · Social context · Trust
Abstract
The paper explains how subjective well-being can be measured, how the resulting data are being used to document human progress and how health care can be changed to take advantage of what has been learned. The evaluations that people make of their own lives document, and permit the explanation of, life satisfaction levels that differ greatly among countries and communities. Research seeking to ex- plain these happiness differences, and their related differences in mortality and morbidity, exposes the importance of the social context. There is an opportunity and need to change health care from the diagnosis and treatment of illness to the fostering of wellness. The importance of the social context in the successful design and delivery of health and happiness is so great as to support a prescription to turn the “I” into “we,” thereby turning illness into wellness by making the production and maintenance of health and happiness a much more collaborative activity, even in the presence of the increasing complexity of medical science.
Introduction
The idea of using happiness as a focal point for policy has emerged in parallel with growing dissatisfaction [1] with using production of goods and services (the most usual measure being Gross Domestic Product, or GDP, per capita) as a sufficient measure of human progress. The choice of happiness as a more encompassing measure of the quality of life has been fueled by decades of research aimed at creating a transdisciplinary science of happiness. These converging threads came together on July 19, 2011, when the United Nations General Assembly adopted a Bhutan-sponsored resolution that “called on United Nations Member States to undertake steps that give more importance to happiness and well-being in determining how to achieve and measure social and economic development” (https://news.un.org/en/story/2011/07/382052).
That resolution led to a “High-Level Meeting on Well-Being and Happiness: Defining a New Economic Paradigm,” convened by the Prime Minister of Bhutan, at the United Nations on April 2, 2012. The meeting marked the release of the first World Happiness Report, which presented the available global data on national happiness and reviewed related evidence from the emerging science of happiness. That report, and the underlying research, provided strong support for the view that the quality of people’s lives can be coherently, reliably, and validly assessed by a variety of subjective well-being measures, collectively referred to in this report as “happiness.”
The first two main sections of this paper first review ways of measuring subjective well-being and a number of key determinants, while the third sketches the implications of these results for how health care might be designed and delivered so as to contribute to happiness.
Measuring Population Well-Being
Life evaluations have been granted a central role in the World Happiness Reports because they provide an umbrella measure by which the relative importance of the supporting pillars for good lives can be compared. The subsequent Guidelines on Measuring Subjective Well-Being developed by the Organization for Economic Cooperation and Development [2] also emphasized the need to measure life evaluations as a primary indicator, ideally in concert with monitoring affect (i.e., the frequency of feelings, states and emotions, both positive and negative) and “eudaimonia” (i.e., measures of life purpose). The guidelines also discuss the need to consider other factors that have been found to support better lives (e.g., income, health, good jobs, family and friends, welcoming communities, good government, trust, generosity, and a healthy environment). Having an umbrella measure of subjective well-being permits the relative importance of these factors in supporting well-being to be assessed, making it possible to move beyond a general wish to improve well- being towards establishing a standard for comparison of alternative policies.
Evidence continues to accumulate showing that life evaluations, positive affect, and negative affect, long thought to capture different aspects of subjective well-being [3], are now seen to do so in a consistent manner, so much so as to be used as indicators of national progress [4]. Of these 3 ways of measuring subjective well-being, life evaluations provide the most encompassing indicator of the quality of life. Life evaluations themselves have taken 3 different forms: life satisfaction questions of the sort advocated by the Organization for Economic Cooperation and Development [2], questions asking how happy people are with their lives as a whole, and the Cantril ladder question used in the Gallup World Poll, wherein people are asked to think of their lives as a ladder, with the worst possible life for them as a 0 and the best as a 10. If these different life evaluation questions are asked of the same respondents (life satisfaction and the Cantril ladder in one year of the Gallup World Poll, and both life satisfaction and happy with life regularly in the European Social Surveys), the answers tell structurally equivalent stories about the correlates of a good life, even though the means and shapes of the distributions of the answers differ among the questions [5].
Questions asking about emotions usually relate to a particular time, while emotions, but not life evaluations, are found to vary by time of day and time of week [6]. Al- though positive and negative emotions are less appropriate as overall measures of the quality of life, they are important in several other key ways. First, their short-term nature makes them natural to use as outcome variables in experimental studies. Second, as will be discussed in the next section, the frequency of a number of emotions, and especially positive affect [7], has been found to add to life satisfaction in predicting a number of future health outcomes [8]. Third, positive emotions have been found to contribute directly to life evaluations, much as Aristotle predicted, and supported by research [9], showing that positive emotions encourage individuals to broaden their networks and activities in ways that build their overall satisfaction with life [10]. Thus, at the aggregate level, the frequency of positive emotions adds significantly to explanations of life evaluations, while the presence or absence of negative emotions has no such effect [10, Table 2.1, col. 4].
Measures of subjective well-being, and especially life evaluations or judgments about how happy people are with their lives as a whole, require the design and collection of other social indicators as candidate variables for the explanation of well-being. The relative sizes of the influences discovered then provide a way to establish the relative importance of many different circumstances thought to influence well-being.
Some have argued that it is misleading to use “happiness” as a generic term to cover subjective well-being more generally. While “subjective well-being” is more precise, it simply does not have the convening power of “happiness.” The main linguistic argument for using “happiness” in a broader generic role is that happiness plays two important roles within the science of well-being, appearing once as a prototypical positive emotion and again as part of a cognitive life evaluation question. This double use has sometimes been used to argue that there is no coherent structure to happiness responses. The converse argument made in the World Happiness Reports is that this double usage helps to justify using happiness in a generic role, as long as the alternative meanings are clearly understood and credibly related. Evidence from a growing number of large-scale surveys shows that the answers to questions asking about the emotion of happiness differ from answers to judgmental questions asking about a person’s happiness with life as a whole in exactly the ways that theory would suggest. Answers to questions about the emotion of happiness relate well to what is happening at the moment. Evaluative answers, in response to questions about life as a whole, are supported by positive emotions, as noted above, but are also driven much more than are answers to questions about emotions by a variety of life circumstances, including income, health, and social trust.
Only life evaluations, among the variety of social indicators considered in a recent retrospective survey [11], meet the two primary tests for an encompassing measure.
First, they have good claims to be themselves global assessments of the quality of life, without any further construction or manipulation. Second, since they are primary measures and also encompassing in their scope, they provide the research base for answering the fundamental questions about sources of a better life. To answer these questions, of course, requires the design and measurement of precisely those social indicators that have been the focus of the past 50 years of social indicators research.
Determinants of Subjective Well-Being
The World Happiness Report uses 6 variables to explain roughly three-quarters of the variation across countries and over time in annual national average life evaluations from usually 1,000 respondents to the Gallup World Poll in each of more than 150 countries. These explanatory variables include national averages for GDP per capita, World Health Organization (WHO) measures of healthy life expectancy, and 4 more socially oriented variables. These additional variables are based on average answers to other Gallup World Poll questions: (a) having someone to count on in times of trouble, (b) having a sense of freedom to make key life decisions, (c) trust (as measured by a perceived absence of corruption in government and business), and (d) generosity (as measured by having given money to others in the previous month). Taken together, these variables are the most important correlates of national happiness, even after allowing for their effects that flow through income and healthy life expectancy. For example, it has been calculated that to move all of those variables from the world’s lowest levels to world average levels would raise average life evaluations by almost 2 points on the 0–10 scale, with almost 1.2 points due to having more people with someone to count on in times of trouble. This social support effect alone is more than the estimated impact of the 18-fold increase in GDP per capita required to shift the poorest country to the world average [10]. These estimates of course rely on correlations, and there are many complex feedbacks in play, so that the empirical results are best seen as illustrative rather than definitive, although most of the implied causal channels have been established by more experimental strategies having a clearer causal interpretation.
These same variables are also very important in explaining differences in life satisfaction between individuals. Indeed, the estimated importance of the social context as a determinant of subjective well-being is even greater when estimated from surveys that contain a richer set of social variables than is available in the Gallup World Poll. Individual-level data for most countries show a U-shape in age, with a mid-life low about the age of 50 years. At each age, but especially in mid-life, when conflicting demands pile up, those with better social contexts have much higher life evaluations. This is shown by the effects of being married [12], especially relative to being divorced or separated, by having a workplace superior who is seen as a partner rather than a boss [13], and by having a sense of belonging to the local community. A stronger versus a weaker sense of community belonging has a powerful influence at all ages, but especially for those over 60 years.

Both the extent and nature of time spent with friends and family are important sources of happiness, whether measured by life evaluations or positive affect. There is a steady dose-response life satisfaction benefit of having a larger circle of real friends, although not of online friends [14].
Trust is an important measure of the quality of the social context and is estimated to have significant effects in all areas of life. For example, a change of 1 point on a 10-point scale for trust in management at one’s work- place is equivalent, in life satisfaction terms, to a 30% change in income [15]. Trust also increases resilience, such that the large happiness reductions suffered by those who are in ill-health, subject to discrimination, or unemployed are significantly less for those who feel that others can be trusted [16].
Generosity is another often ignored support for happiness. Correlational and experimental studies alike have shown that giving either money or care to others raises happiness [17]. Studies of the happiness gains from generosity have shown gains to be larger when the generosity facilitates and accompanies social connection, when it is done for altruistic rather than selfish motivations, when the generous acts are freely done of one’s own volition, and when the acts are felt to make an effective and positive impact on the lives of others [18]. Although there is an established positive feedback loop between generosity and happiness [19], experimental evidence shows a causal link from generosity to happiness even for toddlers, who smile more when they give away a treat than when they consume it themselves [20].
Nutrition enters the picture via a Gallup World Poll question asking whether the respondent has in the past 12 months not had enough money to buy needed food. Variations across individuals or across countries in this measure of food security affect happiness significantly, even when income differences are controlled for [5, Table 10.3].
Implications for Health Care
One way of using research on the determinants of subjective well-being to influence health care is to reform cost-effectiveness analysis to use happiness outcomes as the basic criterion for success [21]. Looking at the consequences of alternative treatments through the lens of happiness leads to more attention being paid to mental health (especially for children [22]), to the better provision of later-life and palliative care, and to a different way of ranking competing elements within health-care budgets. A second way of finding the health consequences of happiness is to assess the extent to which greater levels of affective or evaluative happiness are linked to subsequent health outcomes [23]. Prospective studies have found an association between current happiness and subsequent longevity that seems to be generally stronger among healthy than unhealthy populations [24], being greatest in studies with the longest duration, such as the well- known study of the longevity of nuns over a 60-year follow-up period [25]. An even longer longitudinal study of a cohort of Harvard undergraduates born in the 1920s did not collect measures of life satisfaction but did measure a number of variables, including especially measures of social support, that have been shown to be strong supports for life satisfaction. That study showed social support to be the most important factor in longevity and health in later life [26], as did a combined companion study including men and women from a broader range of backgrounds, over an evaluation period now well into the tenth decade of the lives of the surviving members of the study cohorts [27].
A third and potentially more important route from happiness research to health care is to consider what treatments could and should be done differently in the light of what has been found about the determinants of happiness. Several of the key results reported in the previous section on the determinants of well-being have implications for health care.
In the light of these results, health care needs to be changed fundamentally from the diagnosis and treatment of illness to the measurement and delivery of wellness. Such a transformation requires major changes in medical practice to build the evidence base required to support such an effective transition for treatment. Depression inventories have been worked and reworked for decades [28] and provide a core of common questions for doctors to ask of their patients [29]. Only in the past decade has there been serious development and psychometric testing of comparable inventories of questions about positive states of mind. Shorter and longer versions of such question inventories have been developed, with answers that have been closely associated with a variety of health outcomes [30]. This is what would be expected in the light of evidence showing that the susceptibility to and severity of responses to variable degrees of experimental exposure to a rhinovirus depended much more on the strength of a subject’s pre-existing positive affect than on the negative affect measures [31]. But thus far, there has been little take-up or even much discussion in general or specialty clinical practices. Without a broader clinical base of evidence, it will be difficult to build the scientific understanding of the two-way linkages between positive states of mind and medical outcomes [7]. To get these measures into clinical practice, they must be seen as of the highest priority.
One recent positive development in clinical practice has been the growing use of “social prescribing,” whereby clinicians and associated nonmedical staff direct patients to community resources and tactics that are likely to improve the social context within which people live [32–37]. Given the primary importance of positive social connections for happiness, increased use of social prescribing is almost sure to be part of a happiness-based clinician’s tool kit. Even within the context of social prescribing, the emphasis currently remains focused on diagnosing and treating illness rather than on creating wellness. For example, a screening tool [38] recommended to improve the implementation of social prescribing measures the patient’s social context primarily in terms of deficits, including violence, street safety, and isolation. But as positive psychology and happiness research continue to show, to remove established risk factors for illness offers a return to stasis rather than opening up new opportunities for patients to enrich lives for themselves and others. Another way of putting this basic point is that social prescriptions should be received by all patients, including those who show none of the symptoms in the depression inventory.
Research shows that people tend to underestimate the happiness benefits, both for themselves and others, of generosity and other positive social connections [39]. This opens up an opportunity for universal social prescribing that might be filled by the physician who inquires after the patient’s social context, including at home, in the workplace, the neighborhood, and the community at large. However positive the responses, the physician could underline the health-supporting nature of these positive connections, emphasize their ability to improve the lives of others, and pass along links to further opportunities to enjoy and contribute to local organizations. There is an example in the area of children’s nutrition, where it has been found that the Healthy Start food program in the United Kingdom fails to reach a number of its intended beneficiaries in part because the program has not been a regular part of the information and advice provided by health-care professionals [40]. The importance of having a sense of freedom in making key life decisions would seem to imply happiness ad- vantages for operating a health-care system so that patients are informed and engaged. This could be achieved by better information availability and exchange, a feeling that different elements of the health-care team, including the patients themselves, were working together rather than at cross-purposes, along with the ability to make their own decisions about the form and duration of late-life care. This goes far beyond the points made earlier about the nature of palliative and end-of-life care; in happiness terms, it has more to do with the quality of life for those still living [41]. For example, research in a UK elder care facility showed that residents who were asked to design their own social spaces in a move to a new facility were subsequently happier and healthier, and used the new facilities more, than their peers who had the supposed benefits of access to a professionally designed space [42].
The importance of the social context, and of doing things with others, suggests that happiness benefits from group activities, whether related to regime maintenance, fitness, or simply social engagement. Although much of the related research on the happiness effects of social connections focuses on adults, they have also been documented for young children [43]. Experimentally induced group activities have been found to deliver health benefits [44], spouses who improve their health behavior at the same time are more likely to achieve and maintain the gains [45], and even doing hard physical training in unison rather than independently delivers better performance, measured by pain thresholds [46].
Finally, there is growing evidence that the social context within the health-care environment is a first-order determinant of the happiness of health-care workers and patients and of clinical effectiveness. There is thus a likely application within health care of the results found more generally in the workplace, that happier employees and work teams are also more productive ones [47]. There is some evidence, for example, that in places where the WHO surgical guidelines have improved outcomes, the key channels are related to teamwork and communication in the operating room and are driven importantly by the flattening of hierarchy implied by the preoperative introductions and the mask-free timeout [39].
Conclusion
Whether across nations or among individuals within a society, subjective well-being is determined by the circumstances of life, and especially by the social context in which people live. Morbidity and mortality are also deter- mined by these same factors, both directly and mediated by happiness. These results suggest that health care needs to be changed fundamentally from the diagnosis and treatment of illness to the measurement and delivery of wellness. Such a transformation needs to be informed by an expanded evidence base that gives the measurement and monitoring of positive outcomes a central place.
References
1 Stiglitz JE, Sen A, Fitoussi JP. Report by the commission on the measurement of economic performance and social progress. Available from: https://ec.europa.eu/eurostat/documents/118025/118123/Fitoussi+Commission+report
2 Organisation for Economic Co-operation and Development (OECD). OECD guidelines on measuring subjective well-being. Paris: OECD Publishing; 2013.
3 Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: three decades of progress. Psychol Bull. 1999 Mar;125(2):276–302.
4 Diener E. Subjective well-being. The science of happiness and a proposal for a national index. Am Psychol. 2000 Jan;55(1):34–43.
5 Helliwell JF, Barrington-Leigh C, Harris A, Huang H. International evidence on the social context of well-being. In: Diener E, Helliwell JF, Kahneman D, editors. International differences in well-being. Oxford: Oxford University Press; 2010. pp. 291–327.
6 Helliwell JF, Wang S. Weekends and subjective well-being. Soc Indic Res. 2014 Apr; 116(2):389–407.
7 Cohen S, Pressman SD. Positive affect and health. Curr Dir Psychol Sci. 2006 Jun;15(3): 122–5.
8 De Neve JE, Diener E, Tay L, Xuereb C. The objective benefits of subjective well-being. In: Helliwell J, Layard R, Sachs J, editors. World Happiness Report 2013. New York: UN Sustainable Development Solutions Network; 2013. pp. 54–79.
9 Fredrickson BL. The broaden-and-build theory of positive emotions. Philos Trans R Soc Lond B Biol Sci. 2004 Sep;359(1449):1367–78.
10 Helliwell JF, Huang H, Wang S. The social foundations of world happiness. In: Helliwell J, Layard R, Sachs J, editors. World Happiness Report 2017. New York: UN Sustainable Development Solutions Network; 2017. pp. 8–47.
11 Land KC, Michalos AC. Fifty years after the social indicators movement: Has the promise been fulfilled? Soc Indic Res. 2018 Feb;135(3): 835–68.
12 Grover S, Helliwell JF. How’s life at home? New evidence on marriage and the set point for happiness. J Happ Stud. 2019 Feb;20(2): 373–390.
13 Helliwell JF, Norton MB, Huang H, Wang S. Happiness at different ages: The social context matters. NBER Working Paper. 2018 Oct: 25121.
14 Helliwell JF, Huang H. Comparing the happiness effects of real and on-line friends. PLoS One. 2013 Sep;8(9):e72754.
15 Helliwell JF, Huang H. Well-being and trust in the workplace. J Happ Stud. 2011 Oct; 12(5):747–67.
16 Helliwell JF, Huang H, Wang S. New evidence on trust and well-being. In: Uslaner E, editor. The Oxford Handbook of Social and Political Trust. Oxford: Oxford University Press; 2016. pp. 409–46.
17 Aknin LB, Barrington-Leigh CP, Dunn EW, Helliwell JF, Burns J, Biswas-Diener R, et al. Prosocial spending and well-being: cross-cultural evidence for a psychological universal. J Pers Soc Psychol. 2013 Apr;104(4):635–52.
18 Helliwell JF, Aknin LB, Shiplett H, Huang H, Wang S. Social capital and prosocial behavior as sources of well-being. In: Diener E, Oishi S, Tay L, editors. Handbook of well-being. Salt Lake City, UT: DEF Publishers; 2018.
19 Isen AM, Levin PF. Effect of feeling good on helping: cookies and kindness. J Pers Soc Psychol. 1972 Mar;21(3):384–8.
20 Aknin LB, Hamlin JK, Dunn EW. Giving leads to happiness in young children. PLoS One. 2012;7(6):e39211.
21 Peasgood T, Foster D, Dolan P. Priority set- ting in healthcare through the lens of happiness. In: Global Happiness and Well-Being Policy Report. 2019. Available from: http:// www.happinesscouncil.org
22 Layard R, Hagell A. Healthy young minds: Transforming the mental health of children. In: Helliwell JF, Layard R, Sachs J, editors. World Happiness Report 2015. New York: Sustainable Development Research Network; 2015. pp. 106–31.
23 Steptoe A. Happiness and Health. Annu Rev Public Health. 2019 Jan;40(1):annurev-publ- health-040218-044150.
24 Veenhoven R. Healthy happiness: effects of happiness on physical health and the consequences for preventive health care. J Happ Stud. 2008 Sep;9(3):449–69.
25 Danner DD, Snowdon DA, Friesen WV. Positive emotions in early life and longevity: findings from the nun study. J Pers Soc Psychol. 2001 May;80(5):804–13.
26 Vaillant GE, Meyer SE, Mukamal K, Soldz S. Are social supports in late midlife a cause or a result of successful physical ageing? Psychol Med. 1998 Sep;28(5):1159–68.
27 Vaillant GE. Aging well: Surprising guide-posts to a happier life from the landmark Harvard study of adult development. Little, Brown and Company; 2002.
28 DSM-5 Task Force. Diagnostic and statistical manual of mental disorders (DSM-5). Arlington, VA: American Psychiatric Association; 2013.
29 Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 Nov;282(18):1737–44.
30 Su R, Tay L, Diener E. The development and validation of the Comprehensive Inventory of Thriving (CIT) and the Brief Inventory of Thriving (BIT). Appl Psychol Health Well- Being. 2014 Nov;6(3):251–79.
31 Cohen S, Doyle WJ, Turner RB, Alper CM, Skoner DP. Emotional style and susceptibility to the common cold. Psychosom Med. 2003 Jul-Aug;65(4):652–7.
32 Benson T, Sladen J, Liles A, Potts HW. Personal Wellbeing Score (PWS) – a short version of ONS4: development and validation in social prescribing. R-Outcomes Research Paper 17/03 v2. 2018.
33 Bickerdike L, Booth A, Wilson PM, Farley K, Wright K. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017 Apr;7(4):e013384.
34 Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. Br J Gen Pract. 2009 Jun;59(563):454–6.
35 Mercer SW, Fitzpatrick B, Grant L, Chng NR, O’Donnell CA, Mackenzie M, et al. The Glasgow ‘Deep End’ Links Worker Study Protocol: a quasi-experimental evaluation of a social prescribing intervention for patients with complex needs in areas of high socioeconomic deprivation. J Comorb. 2017 Jan;7(1):1–10.
36 Oldman C. The benefits of social prescribing. J Health Visiting. 2016 Jun;4(6):326.
37 Pilkington K, Loef M, Polley M. Searching for real-world effectiveness of health care innovations: scoping study of social prescribing for diabetes. J Med Internet Res. 2017 Feb; 19(2):e20.
38 Gottlieb L, Cottrell EK, Park B, Clark KD, Gold R, Fichtenberg C. Advancing social prescribing with implementation science. J Am Board Fam Med. 2018 May-Jun;31(3):315– 21.
39 Helliwell JF, Aknin LB. Expanding the social science of happiness. Nat Hum Behav. 2018 Feb;2:248–252.
40 Lucas PJ, Jessiman T, Cameron A, Wiggins M. Healthy Start in England: messages for health professionals. J Fam Health Care. 2013 May; 23(4):12–5.
41 Gawande A. Being mortal: medicine and what matters in the end. London: Metropolitan Books; 2014.
42 Knight C, Haslam SA, Haslam C. In home or at home? How collective decision making in a new care facility enhances social interaction and wellbeing amongst older adults. Ageing Soc. 2010 Nov;30(8):1393–418.
43 Holder MD, Coleman B. The contribution of social relationships to children’s happiness. J Happ Stud. 2009 Jun;10(3):329–49.
44 Haslam C, Cruwys T, Haslam SA, Dingle G, Chang MX. Groups 4 Health: evidence that a social-identity intervention that builds and strengthens social group membership improves mental health. J Affect Disord. 2016 Apr;194:188–95.
45 Jackson SE, Steptoe A, Wardle J. The influence of partner’s behavior on health behavior change: the English Longitudinal Study of Ageing. JAMA Intern Med. 2015 Mar;175(3): 385–92.
46 Cohen EE, Ejsmond-Frey R, Knight N, Dun- bar RI. Rowers’ high: behavioural synchrony is correlated with elevated pain thresholds. Biol Lett. 2010 Feb;6(1):106–8.
47 Krekel C, Ward G, De Neve JE. Employee well-being, productivity and firm performance: Evidence and case studies. In: Global Happiness and Well-Being Policy Report. 2019. Available from: http://www.happiness-council.org