Breastfeeding, Childhood Asthma, and Allergic Disease
Key Messages
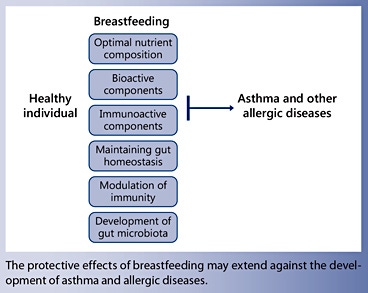
- Breastfeeding may protect against the development of asthma and allergic disease in children, although this topic has been controversial for more than 8 decades.
- Breastfeeding is recommended for at least the first 6 months of life and up to 2 years for immunological development of the infant.
- Breastfeeding may influence immune responses through the bioactive, immune-modulating properties of breast milk, or through the impact of milk type on intestinal microbiota.
- The composition of breast milk cytokines deserves further investigation, because cytokines may provide protection against wheeze and subsequent asthma in childhood.
Key Words
Breastfeeding · Allergic disease · Childhood asthma
Abstract
The worldwide prevalence of childhood asthma has been increasing considerably, and the protection afforded by breastfeeding in its development has been the subject of controversy for more than 80 years. Previous systematic reviews have generally found a protective effect of breastfeeding on allergic outcomes, although many studies have methodological limitations. Although breastfeeding is protective against lower respiratory tract infection during infancy, such protection has not been demonstrated for asthma in all studies. Breastfeeding has health benefits for the mother and child. Exclusive breastfeeding for the first 6 months of an infant’s life, with continued breastfeeding for up to 2 years or longer, is recognized as the “gold” standard for infant feeding because human milk is uniquely suited to the human infant, and its nutritional content and bioactivity promote a healthy development. There is increasing concern that the practice of delaying complementary foods until 6 months may exacerbate the risk of allergic disease. Breast milk contains immunological components that protect against infections and allergic disease in infancy. The composition of human breast milk is complex, containing factors that interact with the infant immune system and intestinal milieu including allergens, cytokines, immunoglobulins, polyunsaturated fatty acids, and chemokines. Transforming growth factor β is a cytokine in human milk involved in maintaining intestinal homeostasis, inflammation regulation, and oral tolerance development. Modern day society, with increased standards of hygiene, has changed the gut flora of Western infants, potentially impacting the risk of developing immune-mediated diseases including allergic disease and asthma. Microbial diversity is intrinsic to healthy immune maturation and function. Compared to breastfed infants, formula-fed infants had lower bacterial diversity and an altered intestinal microbiota in the first few weeks of life associated with an increased risk of eczema and asthma. Favorable gut colonization through continued breastfeeding may promote tolerance as well as protection when complementary feeding is initiated.
Introduction
Breastfeeding and Childhood Illness
Breastfeeding has numerous health benefits for the mother and child [1]. Exclusive breastfeeding for the first 6 months of an infant’s life, with continued breastfeeding for up to 2 years or longer, is recognized as normal and the “gold” standard for infant feeding [2, 3]. This is because human maternal milk is uniquely suited to the human infant, and its nutritional composition and non-nutritive bioactive factors promote healthy development and ultimately survival. Breast milk contains immune factors such as IgA antibodies protecting against many health problems in infancy, such as necrotizing enterocolitis, overweight and obesity, diabetes, infections, and allergic disease [2, 4], as well as reducing the risk of diseases later in life [5].
In the past 30 years, the evidence for global breastfeeding recommendations has evolved remarkably. Epidemiological studies combined with growing insights from epigenetics, stem cell research, and the “developmental origins of health and disease” hypotheses offer strong and solid support to the concept that breast milk is best for human infants. Never before in science history has so much been known about the complex significance of breastfeeding for mothers and their children.
However, the protection afforded by breastfeeding against the development of childhood asthma and allergic disease has been the subject of controversy in the literature. Although breastfeeding is protective against lower respiratory tract infection during infancy, such protection has not been demonstrated for asthma in all studies. Issues related to study design, analytical methods, and confounding have greatly complicated the interpretation and comparison of studies. Furthermore, asthma has a complex phenotype in which numerous genetic and environmental determinants interact. Consequently, the effect of any single determinant is likely to be small and the independent effects difficult to quantify. Asthma is common at a population level, and breastfeeding is amenable to intervention, so a small effect may have implications for public health. For this reason, it is important to establish whether breastfeeding modifies the risk of childhood asthma, even if the effect is small.
Against this background of breast milk significance, there is evidence that breastfeeding may protect against the development of asthma and allergic disease in children although this has been controversial since it was first observed more than eight decades ago [6, 7].
Definition of Infant Feeding
The World Health Organization [8] defines “exclusive breastfeeding” as feeding with breast milk “only” with no other liquid, solids, or vitamin drops. An infant who receives water or juice but not formula is considered “predominantly breastfed,” whereas an infant who receives formula milk, if only for one feed, is considered “partially breastfed,” and “never breastfed” refers to a situation where breastfeeding was never initiated. Thereafter, to meet their evolving nutritional requirements, infants should receive nutritionally adequate and safe complementary foods while breastfeeding continues for up to 2 years of age or beyond [9].
Definition of Allergic Disease
The definitions of allergic disease are varied and inconsistent across studies. For example, different studies have used allergen sensitization, self-report, or doctor diagnosis to define presence of food allergy, with the first two definitions correlating poorly with food challenge for diagnosis of food allergy (the gold standard). Similarly, diverse outcome definitions have been applied in studies evaluating the impact of breastfeeding on eczema, asthma, and allergic rhinitis [4].
To limit the scope of this review, the focus is largely on asthma. Asthma represents a chronic, complex, polygenic interaction in individuals with varying environmental exposures [10]. Asthma is the most chronic disease of childhood and the leading cause of morbidity in children globally as measured by emergency department visits, hospitalizations, and days of missed school [11, 12]. Childhood asthma prevalence worldwide has been increasing over decades, and a number of theories are proposed to explain this startling trend. An overview of current thinking in relation to the breastfeeding, asthma, and allergic disease debate is given – from epidemiological, nutritional, immunological, and gut microbial colonization perspectives.
Determinants of Childhood Asthma and Allergic Disease
The disease has a broad spectrum of possible determinants extending from genetics to lifestyle to environmental factors. Environmental allergens such as smoking in the household, house dust mite, grasses, or pollens may be implicated. Lifestyle and environmental factors including obesity, living in an urban environment, dietary patterns including fast food and poor diet quality, formula milk feeding, gut flora imbalance, smoking, pollution, and infection (viral) have been associated with asthma exacerbations in childhood [12]. Susceptibility to asthma may be increased by early life factors including low birthweight, preterm birth, young maternal age, and male gender. On the other hand, early exposure to respiratory infections may protect, although certain infections may increase the risk [13]. Breastfeeding is implicated because it has been shown to protect against early respiratory and other infections [14].
Epidemiological Studies on Breastfeeding, Asthma, and Allergic Disease
Epidemiological studies in the debate as to whether breastfeeding can have a role in protecting against allergic disease and asthma in early childhood provide conflicting results. While breastfeeding is recommended for all infants irrespective of allergic heredity [15], with protective effects of breastfeeding on asthma reported in young children [16–18], other studies of children at high [19, 20] or low risk [21] or adults [22, 23] show no protective effects.
Systematic Reviews
Previous systematic reviews have found a protective effect of breastfeeding on allergic outcomes, although most studies have methodological limitations, such as heterogeneity or noncompliant standards. A recent review and meta-analysis aimed to identify and summarize publications on breastfeeding and childhood asthma risk in the general population as well as stratify analyses and meta-regression to explore sources of heterogeneity [24]. Compared with other reviews, this review includes a large number of studies, restricts search and study selection minimally, and includes studies of different methodologies, operational definitions for breastfeeding and asthma, and sets of confounders [24]. These criteria may have increased the variability of effect estimates. Limitations were overcome by performing meta-analyses in standardized subgroups and meta-regressions with a broad array of predictors. An assessment of the methodological quality of the studies using criteria based on Kramer’s standards [25] was made and a score based on these criteria was included in the analyses, which addressed heterogeneity between studies. The authors of this review found evidence that children breastfed longer have a lower risk for developing asthma (Fig. 1). Risk reduction was pronounced in children 0–2 years of age, decreasing with age, but still evident at school age with greater effects in early life supporting the theory of protection from early infection. Studies were highly heterogeneous, and results were similar when only longitudinal cohort studies or studies of high methodological quality were included.
Few studies have attempted to assess the association of breastfeeding over the spectrum of allergic conditions: asthma, eczema, allergic rhinitis, and food allergy, which is important because of the substantial overlap in allergic diseases with shared phenotypes. The systematic review of Lodge et al. [26] aimed to analyze current evidence through proven search methods, investigate the heterogeneity and quality of included studies, and contextualize results with respect to the findings related to breastfeeding and allergic outcomes. In this review of various study types, weak evidence that breastfeeding is protective for allergic disease is evident. In spite of heterogeneity in the studies of this review, there is strong evidence that breastfeeding is associated with a reduced risk of asthma (Fig. 2).
Studies were further grouped into those reporting eczema up to or beyond 2 years [26] (Fig. 3). A reduced risk of eczema below 2 years was observed after pooling 6 cohort study estimates comparing exclusive breastfeeding for more than 3–4 months with other feeding types (re OR 0.74, 95% CI 0.57–0.97, I2 62%). Weak evidence that breastfeeding reduced the risk of eczema up to 2 years was observed.
A review that included all study types published in 2011 considering breastfeeding and wheezing illness beyond 5 years of age only showed no association, highlighting an enormous controversy in this area [27] . The authors of this review recommend that further studies should aim to be of the highest quality and specific diagnostic criteria for asthma to be included.
A Birth Cohort “Case” Study
One cohort study assessed the association between breastfeeding and asthma from 1 to 8 years and found that breastfeeding for more than 4 months was associated with significantly reduced asthma prevalence regardless of family history and without evidence of attenuation [28]. The study population, 3,963 Dutch children born in 1996/1997 participating in the PIAMA birth cohort study, was followed for 8 years. Asthma was defined as at least one attack of wheeze and/or dyspnoea and/or prescription of inhalation steroids in the previous 12 months. Chronic asthma was defined as asthma diagnosis at 8 years with asthma diagnosis in at least 2 other years. Specific IgE to common airborne allergens and bronchial hyperresponsiveness were measured according to a standard protocol [29]. Breastfeeding was defined as the duration of any breastfeeding (no breastfeeding, breastfeeding for 1–16 weeks, breastfeeding for more than 16 weeks). “Generalized estimating equation” modelling was applied to test for associations between breastfeeding and repeated respiratory outcomes until 8 years adjusting for gender, maternal education, smoking during pregnancy, and current smoking and stratified by parental allergy. Because 10% of baseline data were missing, missing data were imputed. Final imputation, however, made no difference to the study findings.
In this study, asthma risk was shown to be lower in children breastfed for more than 16 weeks compared to those not breastfed [28]. Children breastfed for the longer duration had significantly fewer chronic asthma symptoms. Having an allergic or nonallergic mother did not change these associations. Breastfeeding for more than 16 weeks was inversely associated with sensitization to airborne allergens at 8 years with no association observed for bronchial hyperresponsiveness. Breastfeeding was associated with a lower asthma risk at all years regardless of parental history. Repeated measures analysis showed a lower risk of wheeze and asthma from 1 to 8 years in babies breastfed for a longer duration, suggesting that breastfeeding affects long-term outcomes. Strengths of the study include longitudinal design, follow-up until 8 years, repeated measures of data collection, a large study population, low attrition rate, and multiple imputation. The birth cohort design with longitudinal analysis allowed demonstration that breastfeeding protects against asthma throughout childhood both with and without a family history and contributing significantly to the breastfeeding and childhood asthma debate.
How May Breastfeeding Protect against Allergic Disease?
Timing of Introduction of Solids There is increasing concern that the current practice of delaying complementary foods to 6 months of age may exacerbate the risk of immune disorders such as eczema and allergic disease. In addition, evidence suggests that favorable gut colonization through continued breastfeeding may promote tolerance as well as protection when complementary feeding is initiated. Conflict exists between some allergy prevention guidelines that currently recommend delaying the introduction of allergenic foods until at least >12 months, whereas the new recommendations are for the introduction of allergenic foods between 4 and 6 months [30] and not before 6 months [9]. Prescott et al. [31] suggested that early introduction of certain allergenic foods is safe and may build tolerance. Other researchers support the hypothesis that later introduction of foods increases allergenic responses [32]. Koplin et al. [32] showed, following adjustment for confounding, that a later introduction to egg increased rates of egg allergy (OR 3.4, 95% CI 1.8–6.5, at >12 months) compared to introducing egg between 4 and 6 months. These results have major implications for practice and future research as they suggest that the introduction of cooked egg at 4–6 months of age may protect against egg allergy and that delaying introduction to egg may exacerbate it. Confirmation of these findings may result in strong changes to infant feeding guidelines, which currently recommend delaying the introduction of allergenic foods until at least >12 months.
The prevalence of peanut allergy among children in Western countries has doubled in the past 10 years, and therefore a study to evaluate strategies in preventing the development of peanut allergy in infants at high risk for the allergy was conducted [33] . The early introduction of peanut significantly decreased peanut allergy development among high-risk children and modulated immune responses to peanuts. In response to these findings, guidelines have recently changed in relation to peanut allergy in the United States [34].
Bioactive Components in Milk
Breastfeeding protects against wheeze in infancy [14], and several components of human milk have been postulated as conferring this protective effect [35]. Protection may be through a myriad of factors in milk including bioactive enzymes, hormones, growth factors, cytokines, and immunological agents. These findings augment and stimulate host defense development [36, 37], suggesting that bioactive components of milk are important in neonatal development and biologically plausible mechanisms through breastfeeding may impact asthma etiology. Breastfeeding has been associated with protection against early respiratory infections [13], and the observed association between breastfeeding and asthma at early ages may be mediated by the protection of breastfeeding against infections. Breastfeeding may provide an immediate line of defense against infectious agents, compensating directly for immaturity of the newborn immune system in its ability to resist infection [38]. However, it is not clear which components of this complex biological fluid account for any potential protective effect.
The Composition of Breast Milk
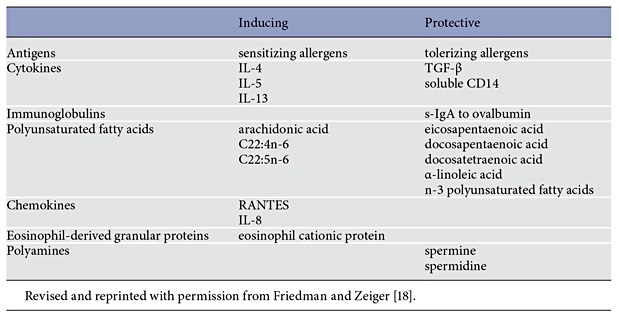
One of the reasons that studies of breastfeeding and allergic disease remain inconclusive could be the complexity of interaction between breast milk, the infant intestinal milieu, and the developing immune system. Some elements in breast milk may protect the infant from developing allergies, whereas others may act in an opposing way (Table 1).
The components of breast milk have immunomodulatory activity, including antigens (allergens), cytokines, immunoglobulins, polyunsaturated fatty acids, and chemokines [18]. It is known that secretory IgA (s-IgA) is passed from mother to infant through breast milk or colostrum. s-IgA may confer passive protection to the infant immune system. Low levels of s-IgA in breast milk are associated with an increased risk of cow’s milk allergy in infants. Lower s-IgA levels to ovalbumin have been shown in colostrum and mature milk of allergic mothers compared to mothers without allergy, although the presence of these antibodies was not predictive of allergies in their infants [39].
Cytokines
Cytokines are small soluble glycoproteins acting in an autocrine-paracrine fashion by binding to specific cellular receptors, operating in networks, and orchestrating immune system development and function [40]. Human milk was revealed to contain cytokines more than 20 years ago [41], and early milk has an abundance of cytokines at a time when neonatal organ systems are immature.
Cytokine concentrations may play a role in breast milk immunogenicity. IL-4, IL-5, and IL-13 cytokines intimately involved with IgE production and eosinophil induction exist in higher concentrations in breast milk of atopic mothers compared with nonatopic mothers. Soluble CD-14 may protect against allergy development due to its high concentrations in breast milk and importance in the TH1 induction response to bacteria [42].
Transforming Growth Factor-β
Transforming growth factor-β (TGF-β) is a cytokine identified in human milk [43], containing TGF-β1, TGF-β2, and other isoforms at mRNA and protein levels with TGF-β2 being the major isoform (95%) [44]. The immunoactive factors in breast milk may influence the development and maturation of the mucosal immune system of the infant [45–50], and mounting evidence suggests that TGF-β, a multifunctional polypeptide, may be a key immunoregulatory factor for the establishment of this response, by promoting IgA production as well as induction of oral tolerance [44, 49, 51–54]. TGF-β increases the infant’s ability to produce IgA against β-lactoglobulin, casein, gliadin, and ovalbumin [44]. In an infant prone to cow’s milk allergy, an increased TGF-β content of mother’s milk may be beneficial by promoting IgG-IgA antibody production and inhibiting IgE- and cell-mediated reactions to cow’s milk [39, 54].
Original work [55, 56] showed that TGF-β1 was a growth factor exhibiting pleiotropic regulatory effects on developmental and physiological pathways. Disruption of the TGF-β1 gene by homologous recombination in murine embryonic stem cells generated mice that carry the disrupted allele. Homozygotic animals for the mutated TGF-β1 allele showed no gross developmental abnormalities about 20 days after birth, but they then succumbed to a wasting syndrome with a multifocal, mixed inflammatory cell response and tissue necrosis leading to organ failure and death [55]. Letterio et al. [49] observed that TGF-β-deficient mice survived while breastfeeding (i.e., TGF-β1 gene knockout), indicating that maternal sources of TGF-β1 via both placental transfer and milk are essential for normal development and postnatal survival.
The role of milk-borne TGF-β in exposed lactating mice to an airborne allergen assessed the development of asthma in progeny. Breastfeeding-induced tolerance relied on the presence of TGF-β during lactation, was mediated by regulatory CD4+ T lymphocytes, and was dependent on TGF-β signaling in T cells [57]. Airborne allergens transferred from mother to newborn through breast milk induced antigen-specific tolerance in the offspring resulting in protection against allergic disease. Breast milk-mediated transfer of an antigen and TGF-β to the neonate resulted in oral tolerance induction and antigenspecific protection from allergic disease. Further, oral administration of TGF-β in vivo in animal studies results in biological activity sufficient to promote oral tolerance [58].
New insights into the mechanisms underlying tolerance induction in neonates pinpoint maternal influence through “breast milk-mediated antigen transfer” as crucial in the process. Because the amount of TGF-β in maternal milk is less in mothers with atopic disease [59–61], these and other findings [48] suggest that this milk cytokine may influence the development of allergic disease and asthma.
The publication of these reviews relating to TGF-β regulation to immune responses [62, 63] and other studies highlight the importance of milk TGF-β [64], although the mechanistic pathways by which TGF-β modulates development and maintenance of the immune system and its role in regulation of tolerance and immunity has not yet been fully described.
Probiotics
The administration of probiotics may increase human milk TGF-β concentration depending on the probiotic strain. Inverse effects have been seen with Lactobacillus reuteri [65], and because concentrations of human milk TGF-β may be critical in determining immune function, more work is needed in this area.
Case Study: Infant Immune Study
Data on breastfeeding and infant wheeze were collected from birth to 1 year from 243 mothers as part of the Infant Immune Study in Tucson, AZ, USA [66]. Breast milk samples obtained at 11 days postpartum (mean age) and assayed by ELISA for concentrations of TGF-β1, IL- 10, TNF-α, and soluble form of CD14 as well as cytokine dose and its relationship with wheeze were assessed. An increasing duration of breastfeeding was associated with decreased prevalence of wheeze (p = 0.039). A higher TGF-β1 dose was associated with less wheeze (p = 0.017) at 1 year, showing a linear trend with wheeze (χ2 p = 0.006) when considered as a dose ( Fig. 4 ). The risk of wheeze decreased (OR 0.22, 95%CI 0.05–0.89, p = 0.034) with increasing dose of TGF-β1 (identified from longer duration of breastfeeding and TGF-β1 concentration level, as compared to short duration of breastfeeding and low TGF-β1 concentration level) when adjusted for sex, gestational age, maternal smoking, exposure to other children, maternal education, and maternal asthma. The dose of TGF-β1 from breast milk had a significant relationship with infant wheeze at 1 year. Because wheeze is a risk factor for asthma in childhood, this relationship is significant.
The authors concluded that TGF-β from human milk is a family of growth factors involved in maintaining intestinal homeostasis, inflammation regulation, allergy development, and promotion of oral tolerance development. The dose of human milk TGF-β1 and TGF-β2 may modulate or regulate immunological responses of infants in early postnatal life. The composition of breast milk cytokines deserves further investigation, because cytokines may provide protection against wheeze and subsequent asthma in childhood.
Polyunsaturated Fatty Acids and Polyamines
Polyunsaturated fatty acids and polyamines may impact on the allergenicity and/ or immune protectiveness of breast milk. A high arachidonic acid to eicosapentaenoic acid ratio in breast milk may be associated with a higher risk of allergic disease and atopy, although this is controversial [67]. How these various mechanisms of immunomodulation are expressed in mother-infant pairs is not known. Genetic factors may allow better predictability but require future investigation to determine the complex interaction effects of immunomodulatory factors in milk and development of allergic disease [68].
Intestinal Microbiota
Modern day society, with increased standards of hygiene, has changed the gut flora of Western infants, potentially impacting the risk of developing immune-mediated diseases including allergic disease and asthma [69]. In adults, intestinal microbiota consists of several hundred, mostly anaerobic, bacterial species. Formed through successive establishment of different bacteria in infancy and early childhood, this system is complex. Facultative and aerotolerant bacteria establish first, followed by more and more strict anaerobes, and commensal microbes provide major incentive for immune system maturation.
The microbial colonization of the newborn intestine is influenced by delivery and feeding mode, family structure, and other lifestyle behaviors. Gut microbiota are required for normal immune development, regulation of gut inflammatory responses, and oral tolerance induction to new foods [70]. The specific microbial changes associated with protection against allergic disease remain uncertain, and more recent data suggest that microbial diversity may be of relevance [69, 71, 72]. Altered intestinal microbiota in the first few weeks of life is associated with increased risk of eczema and asthma in infancy [7, 73– 75]. Mice raised in a germ-free environment failed to develop oral tolerance and had persistent Th2-dependent responses [76]. This immune deviation may be experimentally corrected by Bacteroides fragilis seeding, but only during the neonatal period.
Breastfeeding for 4–6 months may assist in the development of a healthy gut microbiota by providing bifidobacteria and lactic acid bacteria that reinforce colonization [77] and by supplying galacto-oligosaccharides that promote a healthy microbiota composition. A wide variety of galacto-oligosaccharides are found in breast milk, exhibiting bifidogenic effects in the infant gut. Breast milk also contains nucleotides, IgA, and antimicrobial factors such as lactoferrin, which can modulate the infant gut microbiota composition.
Breastfeeding facilitates the exchange of microbes between mother and infant, and bacterial diversity could be intrinsic to healthy immune maturation and function. Minor differences are seen in microbial content between breast- and formula-fed infants, reflecting improved infant formulas in the past 30 years [69]. Bifidobacteria and lactobacillus are found in both breast- and formula-fed babies, although formula-fed babies have more prevalent and higher counts of Clostridium difficile, Bacteroides, enterococci, and Enterobacteriaceae, while staphylococci are more numerous in breastfed infants. Generally, formula- fed infants had lower bacterial diversity. Further research is required to define the microbial stimulus for normal development, investigate the mechanisms involved, and confirm the role of microbiota in protection for allergic disease.
The Debate Continues
The debate whether breastfeeding protects against allergic disease and asthma in children continues, and it is still not possible to make a definitive conclusion regarding this relationship. Much of the difficulty is in the various study designs applied to ask the question. In addition, other factors impact breast milk and its link to allergic disease, such as the mother’s diet, the infant’s diet, maternal microbiota and exposure to allergens in the environment, timing of introduction to other foods, and composition of the mother’s milk (nutritional, immunomodulatory, bioactive). Many of these factors have not been assessed in studies considering the research question “does breastfeeding impact allergic disease?” Research needs to consider confounding, effect modification, and interactions. More research into the bioactive factors within breast milk (such as TGF-β) is required to identify possible effect modifiers. Finally, exclusive breastfeeding for 6 months continues to be the keystone for the promotion of allergy health and continues to be recommended by international pediatric societies and academies [78, 79].
Disclosure Statement
The author has no conflict of interest to disclose. The writing of this article was supported by Nestlé Nutrition Institute.
References
- Ballard O, Morrow AL: Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am 2013; 60: 49–74.
- American Academy of Pediatrics: Policy Statement: breastfeeding and the use of human milk. Pediatrics 2012; 129:e827–e841.
- World Health Organization Recommendations on Postnatal Care of the Mother and Newborn. Geneva, World Health Organization, 2013.
- Matheson M, Allen KJ, Tang MLK: Understanding the evidence for and against the role of breastfeeding in allergy prevention. Clin Exp Allergy 2012; 42: 827–851.
- León-Cava N, Lutter C, Ross J, Martin L: Quantifying the Benefits of Breastfeeding: A Summary of the Evidence. Washington, Pan American Health Organization, 2002.
- Grulee CG, Sanford HN, Herron PH: Breast and artificial feeding. JAMA 1934; 103: 735.
- Grulee CG, Sanford HN: The influence of breast and artificial feeding on infantile eczema. J Pediatr 1936; 9: 223–225.
- World Health Organization: Indicators for Assessing Infant and Young Child Feeding Practices: Conclusions of a Consensus Meeting Held 6–8 November 2007 in Washington D.C., USA. Geneva, 2008.
- World Health Organization: Global Strategy for Infant and Young Child Feeding. Geneva, 2003.
- Becker A, Chan-Yeung M: Primary asthma prevention: is it possible? Curr Allergy Asthma Rep 2008; 8: 255–261.
- Masoli M, Fabian D, Holt S, Beasley R; Global Initiative for Asthma (GINA) Program: The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004; 59: 469–478.
- Ding G, Ji R, Bao Y: Risk and protective factors for the development of childhood asthma. Paediatr Resp Rev 2015; 16: 133–139.
- Oddy WH, de Klerk NH, Sly PD, Holt PG: The effects of respiratory infections, atopy and breastfeeding on childhood asthma. Eur Respir J 2002; 19: 899–905.
- Oddy WH, Sly PD, de Klerk NH, Landau LI, Kendall GE, Holt PG, et al: Breast feeding and respiratory morbidity in infancy: a birth cohort study. Arch Dis Child 2003; 88: 224– 228.
- Høst A, Halken S, Muraro A, Dreborg S, Niggemann B, Aalberse R, et al: Dietary prevention of allergic diseases in infants and small children. Pediatr Allergy Immunol 2008; 19: 1–4.
- Oddy WH, Holt PG, Sly PD, Read AW, Landau LI, Stanley FJ, et al: Association between breastfeeding and asthma in 6 year old children: findings of a prospective birth cohort study. BMJ 1999; 319: 815–819.
- Gdalevich M, Mimouni D, Mimouni M: Breast-feeding and the risk of bronchial asthma in childhood: a systematic review with meta-analysis of prospective studies. J Pediatr 2001; 139: 261–266.
- Friedman NJ, Zeiger RS: The role of breastfeeding in the development of allergies and asthma. J Allergy Clin Immunol 2005; 115: 1238–1248.
- Wright AL, Holberg CJ, Taussig LM, Martinez FD: Factors influencing the relation of infant feeding to asthma and recurrent wheeze in childhood. Thorax 2001; 56: 192– 197.
- Mihrshahi S, Ampon R, Webb K, Almqvist C, Kemp AS, Hector D, et al: The association between infant feeding practices and subsequent atopy among children with a family history of asthma. Clin Exp Allergy 2007; 37: 671–679.
- Kramer MS, Matush L, Vanilovich I, Platt R, Bogdanovich N, Sevkovskaya Z, et al: Effect of prolonged and exclusive breast feeding on risk of allergy and asthma: cluster randomised trial. BMJ 2007; 335: 815.
- Sears MR, Greene JM, Willan AR, Taylor DR, Flannery EM, Cowan JO, et al: Longterm relation between breastfeeding and development of atopy and asthma in children and young adults: a longitudinal study. Lancet 2002; 360: 901–907.
- Matheson MC, Erbas B, Balasuriya A, Jenkins MA, Wharton CL, Tang ML, et al: Breast-feeding and atopic disease: a cohort study from childhood to middle age. J Allergy Clin Immunol 2007; 120: 1051–1057.
- Dogaru CM, Nyffenegger D, Pescatore AM, Spycher BD, Kuehni CE: Breastfeeding and childhood asthma: systematic review and meta-analysis. Am J Epidemiol 2014; 179: 1153–1167.
- Kramer MS: Does breastfeeding help protect against atopic disease? Biology, methodology, and a golden jubilee of controversy. J Pediatr 1988; 112: 181–190.
- Lodge CJ, Tan DJ, Lau MXZ, Dai X, Tham R, Lowe AJ, et al: Breastfeeding and asthma and allergies: a systematic review and meta-analysis. Acta Paediatrica 2015; 104: 38–53.
- Brew BK, Allen CW, Toelle BG, Marks GB: Systematic review and meta-analysis investigating breast feeding and childhood wheezing illness. Paediatr Perinatal Epidemiol 2011; 25: 507–518.
- Scholtens S, Wijga AH, Brunekreef B, Kerkhof M, Hoekstra MO, Gerritsen J, et al: Breastfeeding, parental allergy and asthma in children followed for eight years: the PIAMA birth cohort study. Thorax 2009; 64: 604–609.
- Burney PG, Luczynska C, Chinn S, Jarvis D: The European Community Respiratory Health Survey. Eur Respir J 1994; 7: 954–960.
- Prescott SL, Tang MLK: The Australasian Society of Clinical Immunology and Allergy position statement: summary of allergy prevention in children. Med J Aust 2005; 182: 464–467.
- Prescott SL, Smith P, Tang M, Palmer DJ, Sinn J, Huntley SJ, et al: The importance of early complementary feeding in the development of oral tolerance: concerns and controversies. Pediatr Allergy Immunol 2008; 19: 375–380.
- Koplin JJ, Osborne NJ, Wake M, Martin PE, Gurrin LC, Robinson MN, et al: Can early introduction of egg prevent egg allergy in infants? A population-based study. J Allergy Clin Immunol 2010; 126: 807–813.
- Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, et al: Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med 2015; 372: 803–813.
- Togias A, Cooper SF, Acebal ML, Assa’ad A, Baker JR Jr, Beck LA, et al: Addendum guidelines for the prevention of peanut allergy in the United States: report of the National Institute of Allergy and Infectious Diseases – sponsored expert panel. J Allergy Clin Immunol 2017; 139: 29–44.
- Field CJ: The immunological components of human milk and their effect on immune development in infants. J Nutr 2005; 135: 1–4.
- Newburg DS, Walker WA: Protection of the neonate by the innate immune system of developing gut and of human milk. Pediatr Res 2007; 61: 2–8.
- Garofalo RP, Goldman AS: Expression of functional immunomodulatory and anti-inflammatory factors in human milk. Clin Perinatol 1999; 26: 361–378.
- Hanson LÅ: Breastfeeding provides passive and likely longlasting active immunity. Ann Allergy Asthma Immunol 1998; 81: 523–537.
- Saarinen KM, Vaarala O, Klemetti P, Savilahti E: Transforming growth factor-β1 in mothers’ colostrum and immune responses to cows’ milk proteins in infants with cows’ milk allergy. J Allergy Clin Immunol 1999; 104: 1093–1098.
- Srivastava MD, Srivastava A, Brouhard B, Saneto R, Groh-Wargo S, Kubit J: Cytokines in human milk. Res Commun Mol Pathol Pharmacol 1996; 93: 263–287.
- Goldman AS, Rudloff HE: Are cytokines in human milk? Adv Exp Med Biol 1991; 310: 93–97.
- Labéta MO, Vidal K, Rey Nores JE, Arias M, Vita N, Morgan P, et al: Innate recognition of bacteria in human milk is mediated by a milk-derived highly expressed pattern recognition receptor, soluble CD14. J Exp Med 2000; 5: 1807.
- Böttcher MF, Jenmalm MC, Garofalo RP, Björkstén B: Cytokines in breast milk from allergic and nonallergic mothers. Pediatr Res 2000; 47: 157–162.
- Kalliomaki M, Ouwehand A, Arvilommi H, Kero P, Isolauri E: Transforming growth factor- beta in breast milk: a potential regulator of atopic disease at an early age. J Allergy Clin Immunol 1999; 104: 1251–1257.
- Goldman AS: Modulation of the gastrointestinal tract of infants by human milk. Interfaces and interactions. An evolutionary perspective. J Nutr 2000; 130: 426S–431S.
- Goldman AS, Chheda S, Garofalo R: Evolution of immunologic functions of the mammary gland and the postnatal development of immunity. Pediatr Res 1998; 43: 155–162.
- Hasselbalch H, Engelmann MD, Ersboll AK, Jeppesen DL, Fleischer-Michaelsen K: Breast-feeding influences thymic size in late infancy. Eur J Pediatr 1999; 158: 964–967.
- Letterio JJ: Murine models define the role of TGF-beta as a master regulator of immune cell function. Cytokine Growth Factor Rev 2000; 11: 81–87.
- Letterio JJ, Geiser AG, Kulkarni AB, Roche NS, Sporn MB, Roberts AB: Maternal rescue of transforming growth factor-beta 1 null mice. Science 1994; 264: 1936–1938.
- Noda K, Umeda M, Ono T: Transforming growth factor activity in human colostrum. Gann 1984; 75: 109–112.
- Ogawa J, Sasahara A, Yoshida T, Sira MM, Futatani T, Kanegane H, et al: Role of transforming growth factor-beta in breast milk for initiation of IgA production in newborn infants. Early Hum Dev 2004; 77: 67–75.
- Savilahti E, Siltanen M, Kajosaari M, Vaarala O, Saarinen KM: IgA antibodies, TGF-beta1 and -beta2, and soluble CD14 in the colostrum and development of atopy by age 4. Pediatr Res 2005; 58: 1300–1305.
- Donnet-Hughes A, Duc N, Serrant P, Vidal K, Schiffrin EJ: Bioactive molecules in milk and their role in health and disease: the role of transforming growth factor-beta. Immunol Cell Biol 2000; 78: 74–79.
- Saarinen KM, Juntunen-Backman K, Jarvenpaa AL, Klemetti P, Kuitunen P, Lope L, et al: Breast-feeding and the development of cows’ milk protein allergy. Adv Exp Med Biol 2000; 478: 121–130.
- Shull MM, Ormsby I, Kier AB, Pawlowski S, Diebold RJ, Yin M, et al: Targeted disruption of the mouse transforming growth factor- beta 1 gene results in multifocal inflammatory disease. Nature 1992; 359: 693– 699.
- Kulkarni AB, Karlsson S: Transforming growth factor-beta 1 knockout mice. A mutation in one cytokine gene causes a dramatic inflammatory disease. Am J Pathol 1993; 143: 3–9.
- Verhasselt V, Milcent V, Cazareth J, Kanda A, Fleury S, Dombrowicz D, et al: Breast milk-mediated transfer of an antigen induces tolerance and protection from allergic asthma. Nature Med 2008; 14: 170–175.
- Ando T, Hatsushika K, Wako M, Ohba T, Koyama K, Ohnuma Y, et al: Orally administered TGF-beta is biologically active in the intestinal mucosa and enhances oral tolerance. J Allergy Clin Immunol 2007; 120: 916– 923.
- Laiho K, Lampi AM, Hamalainen M, Moilanen E, Piironen V, Arvola T, et al: Breast milk fatty acids, eicosanoids, and cytokines in mothers with and without allergic disease. Pediatr Res 2003; 53: 642–647.
- Rigotti E, Piacentini GL, Ress M, Pigozzi R, Boner AL, Peroni DG: Transforming growth factor-β1 and interleukin-10 in breast milk and development of atopic diseases in infants. Clin Exp Allergy 2006; 36: 614–618.
- Oddy WH, Rosales FJ: A systematic review of the importance of milk TGF-beta on immunological outcomes in the infant and young child. Pediatr Allergy Immunol 2010; 21: 47– 59.
- Gorelik L, Flavell RA: Transforming growth factor-beta in T-cell biology. Nature Rev Immunol 2002; 2: 46–53.
- Li MO, Wan YY, Sanjabi S, Robertson AKL, Flavell RA: Transforming growth factor-β regulation of immune responses. Ann Rev Immunol 2006; 24: 99–146.
- Penttila I: Effects of transforming growth factor-beta and formula feeding on systemic immune responses to dietary beta-lactoglobulin in allergy-prone rats. Pediatr Res 2006; 59: 650–655.
- Rautava S: Potential uses of probiotics in the neonate. Semin Fetal Neonatal Med 2007; 12: 45–53.
- Oddy WH, Halonen M, Martinez FD, Lohman IC, Stern DA, Kurzius-Spencer M, et al: TGF-β in human milk is associated with wheeze in infancy. J Allergy Clin Immunol 2003; 112: 723–728.
- Stoney RM, Woods RK, Hosking CS, Hill DJ, Abramson MJ, Thien FC: Maternal breast milk long-chain n-3 fatty acids are associated with increased risk of atopy in breastfed infants. Clin Exp Allergy 2004; 34: 194–200.
- Friedman NJ, Zeiger RS: The role of breastfeeding in the development of allergies and asthma. J Allergy Clin Immunol 2005; 115: 1238–1248.
- Adlerberth I, Wold AE: Establishment of the gut microbiota in Western infants. Acta Paediatr 2009; 98: 229–238.
- Tang MLK: Probiotics and prebiotics: immunological and clinical effects in allergic disease; in Tang MLK, Brandtzaeg P, Isolauri E, Prescott SL (eds): Microbial-Host Interaction: Tolerance versus Allergy. Nestlé Nutr Inst Workshop Ser Pediatr Program. Basel, Karger, 2009, vol 64, pp 219–238.
- Adlerberth I, Strachan DP, Matricardi PM, Ahrné S, Orfei L, Åberg N, et al: Gut microbiota and development of atopic eczema in 3 European birth cohorts. J Allergy Clin Immunol 2007; 120: 343–350.
- Wang M, Karlsson C, Olsson C, Adlerberth I, Wold AE, Strachan DP, et al: Reduced diversity in the early fecal microbiota of infants with atopic eczema. J Allergy Clin Immunol 2008; 121: 129–134.
- Penders J, Thijs C, van den Brandt PA, Kummeling I, Snijders B, Stelma F, et al: Gut microbiota composition and development of atopic manifestations in infancy: the KOALA Birth Cohort Study. Gut 2007; 56: 661– 667.
- Kalliomäki M, Kirjavainen P, Eerola E, Kero P, Salminen S, Isolauri E: Distinct patterns of neonatal gut microflora in infants in whom atopy was and was not developing. J Allergy Clin Immunol 2001; 107: 129–134.
- Bjorksten B, Sepp E, Julge K, Voor T, Mikelsaar M: Allergy development and the intestinal microflora during the first year of life. J Allergy Clin Immunol 2001; 108: 516–520.
- Sudo N, Sawamura S, Tanaka K, Aiba Y, Kubo C, Koga Y: The requirement of intestinal bacterial flora for the development of an IgE production system fully susceptible to oral tolerance induction. J Immunol 1997; 159: 1739–1745.
- Martín R, Olivares M, Marín ML, Fernández L, Xaus J, Rodríguez JM: Probiotic potential of 3 Lactobacilli strains isolated from breast milk. J Hum Lact 2005; 21: 8–17.
- Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Michaelsen KF, et al: Breastfeeding: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2009; 49: 112–125.
- Eidelman AI: Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed Med 2012; 7: 323–324.