A healthy diet is central to overall health throughout the lifecourse and is protective against all forms of malnutrition, as well as non-communicable diseases (NCDs) such as cardiovascular disease, diabetes, obesity, and certain types of cancer. Unhealthy diets and physical inactivity are among the leading causes of NCDs throughout the world and contribute significantly to the global burden of disease, death, and disability. Other conditions related to diet, such as hunger, dental caries, and osteoporosis are widespread causes of morbidity [1].
In the United States, about half of all adults – 117 million individuals – have one or more preventable chronic diseases, many of which are diet-related [2]. More than two-thirds of adults and nearly one-third of children and youth are overweight or obese. These high rates of over- weight, obesity, and chronic disease have persisted for more than two decades and come not only with increased health risks, but also at high cost in terms of personal quality of life and economic and societal costs. The United States spends approximately $400 billion on obesity and diagnosed diabetes-related health costs each year [2]. Many of the risk factors for diet and weight-related diseases are modifiable and preventable.
Healthy dietary patterns associated with positive health benefits are high in vegetables, fruits, whole grains, seafood, legumes, and nuts; moderate in low- and non-fat dairy products; lower in red and processed meat; and low in foods and beverages with added sugars, and refined grains and sodium and provide a balanced caloric intake [2]. Inadequate nutrition, poor diet quality, and obesity are prevalent among all Americans, but are most pronounced among lower-income households and communities, which often lack access to healthy foods or have access to an overabundance of unhealthy foods, as well as in households with limited time to prepare healthful foods.
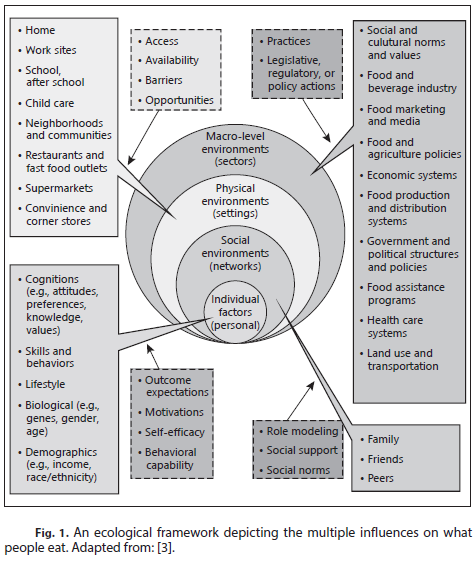
Eating behavior is highly complex, resulting from the interplay of multiple influences across different contexts and conditions. Improving dietary and lifestyle patterns and reducing obesity will require addressing not only individual behaviors but the environmental context and conditions in which people live, make choices, and eat. This work will also require addressing inequities that exist in access to healthy foods and healthy environments more broadly in low-income and disadvantaged communities.
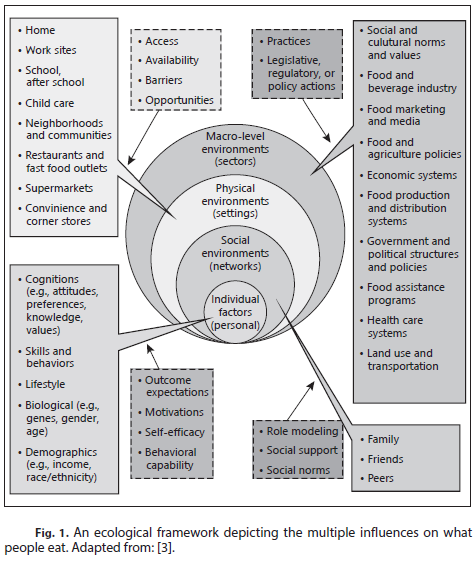
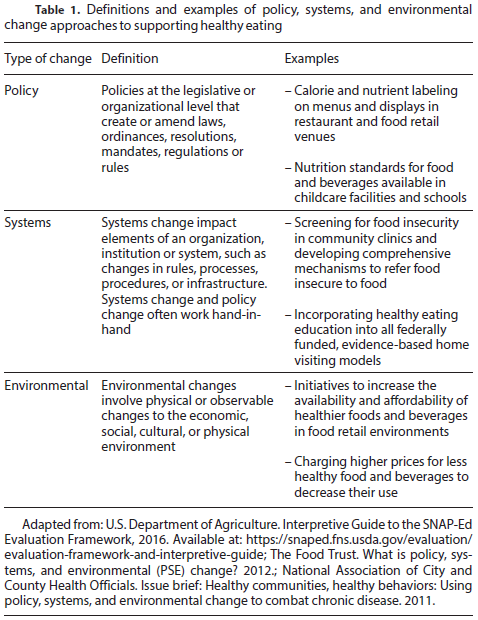
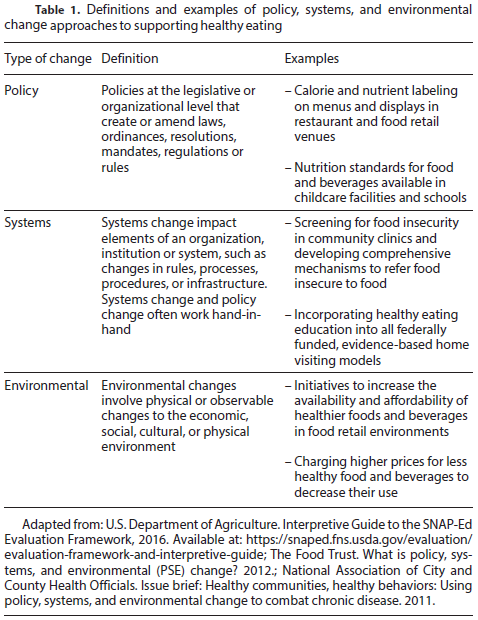
This paper presents a conceptual framework for under- standing the multiple influences on what people eat (Fig. 1) and the linkages between individual-level factors, social environments, physical environments, and macroenvironments [3]. Collectively, these environments influence what, where, and how much we eat. We then discuss policy, systems, and environmental (PSE) dietary change strategies; the goal of which is to make the healthy choice – the easy, safe, and affordable choice and have impact at the population and community level (Table 1). We highlight selected examples of synergistic linkages and interactions between nutrition education and PSE strategies that have proven effective in supporting healthy eating behaviors. Examples include efforts in federal nutrition assistance programs, nutrition and food labeling, and food retail settings. This paper will also explore new sectors where this synergistic approach holds promise for improving population health and reducing health inequities. Accelerating progress in improving healthy eating and dietary quality and achieving and maintaining a healthy weight will require multi-level and multi-sectoral approaches by combining direct nutrition education with broader PSE efforts. To have the greatest population health impact, models that have proven effective should be maintained and new approaches that hold promise for underserved communities should be implemented and evaluated. Nutrition education combined with PSE approaches is more effective than either strategy in isolation and both will be needed to reduce the global burden of diet-related chronic diseases.
References
1. Waxman A; World Health Assembly: WHO global strategy on diet, physical activity and health. Food Nutr Bull 2004;25:292–302.
2. U.S. Department of Health and Human Services and U.S. Department of Agriculture (ed 8). 2015–2020 Dietary Guidelines for Americans. December 2015.
http://health.gov/dietaryguidelines/2015/guidelines.
3. Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K: Creating healthy food and eating environments: Policy and environmental approaches. Annu Rev Public Health 2008:29:253–272