Maternal nutrition plays a critical role in establishing the course of pregnancy and the health of the mother and child at birth and beyond. Current work in the examination of diet with health outcomes focuses on dietary patterns because of the inherent inter-correlation between nutrients and food groups. Recently, the U.S. Department of Agriculture (USDA) and the U.S. Department of Health and Human Services (HHS) initiated the Pregnancy and Birth to 24 Months Project to examine diet- related topics of public health importance during pregnancy, infancy, and toddlerhood [1]. Four systematic review (SR) questions assessed how dietary patterns before and during pregnancy relate to outcomes in mothers and their offspring during the period January 1980 to January 2017 [2]. These outcomes included gestational diabetes (GDM), hypertensive disorders during pregnancy (HDP) (i.e., gestational hypertension, pre-eclampsia, and eclampsia), birth weight, and gestational age (preterm birth, PTB). Evidence on the relationship between diet during pregnancy and GDM was mixed and considered insufficient to draw a conclusion. Five articles examined the association with HDP; the evidence in this review was found to be limited in support of an association between dietary patterns higher in vegetables, fruits, whole grains, nuts, legumes, fish and vegetable oils and lower in meats and refined grains and a reduction in the risk of HDP. For the outcome of PTB, more consistent evidence was found with 5 of the 8 studies that examined the relationship between dietary patterns during pregnancy and overall PTB reporting a significant association. While there were more studies assessing the relationship between dietary patterns and birth weight during pregnancy (n = 17), the evidence was considered inconclusive due to the substantial inconsistency and methodological limitations including a lack of standardization of birth weight for gestational age and sex and no assessment of modification by maternal pre-pregnancy BMI.
There are two additional studies that lend support to the association between dietary patterns and birth outcomes. Martin et al. examined the association between the DASH diet and cardiometabolic markers at mid-pregnancy and found that greater adherence to DASH diet was related to lower maternal fasting glucose, insulin, HOMA-IR, and triglyceride levels with pre-pregnancy BMI attenuating the associations. However, there was no association with total cholesterol levels [3]. The Healthy Start cohort found that a dietary pattern higher in poultry, nuts and seeds, whole grains, cheese, fruits as well as added sugars and discretionary solid fat was positively correlated with maternal gestational weight gain but not mid-pregnancy fasting glucose [4]. Whereas a diet higher in eggs, pota- toes, other starchy vegetables, non-whole grains, fruits (citrus, melons, and berries), and discretionary solid fat was correlated with both gestational weight gain and mid-pregnancy fasting glucose levels.
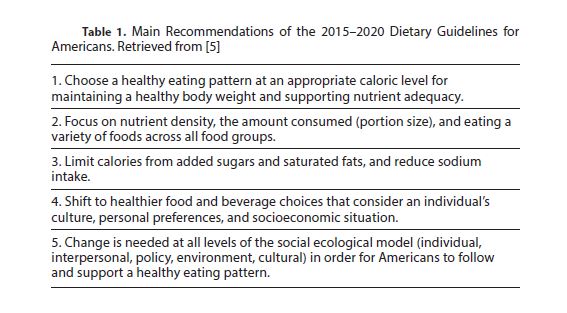
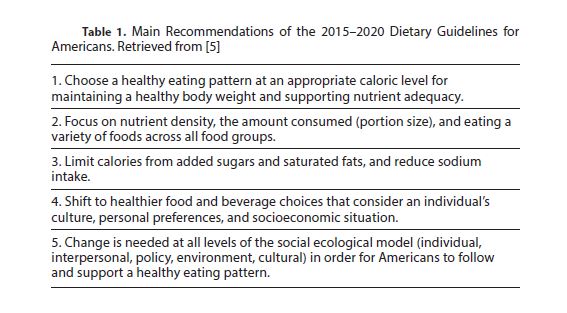
While evidence in support of following specific dietary patterns during pregnancy for an optimal outcome is weak, due to the many methodological limitations of previous studies, there are guidelines that make sense for women to follow. These guidelines include, for example, the healthy dietary patterns included in the 2015-20 Dietary Guidelines for Americans (Table 1) [5]. Key characteristics of these patterns include higher intakes of fish and seafood, vegetables, fruits, whole grains, nuts and seeds, legumes, and vegetable oils.
Maternal weight status, in particular a high BMI (≥30) prior to conception itself, is strongly associated with many adverse birth outcomes. Current gestational weight gain guidelines are dependent on a woman’s starting weight, and intervention studies that have been successful in helping women gain within the target require frequent, high intensity diet counseling. Intervention studies conducted in overweight and obese women show greater heterogeneity in terms of what works, but it seems prudent to provide counseling to these women even through the inter- conceptional period to help mitigate pregnancy complications and child outcomes associated with a high BMI in future pregnancies.
Reference
1. USDA. Pregnancy and Birth to 24 Months Project [Internet] 2018. Available from: https://www.cnpp.usda.gov/birthto24months.
2. USDA. Nutritional Evidence Library (NEL) [Internet] 2018. Available from: https:// www.cnpp.usda.gov/nutritionevidencelibrary.
3. Martin CL, Siega-Riz AM, Sotres-Alvarez D, et al: Maternal dietary patterns are associated with lower levels of cardiometabolic markers during pregnancy. Paediatr PerinatEpidemiol 2016;30:246–55.
4. Starling AP, Sauder KA, Kaar JL, et al: Maternal dietary patterns during pregnancy are associated with newborn body composition. J Nutr 2017;147:1334–1339.
5. US Department of Health and Human Services. 2015-2020 Dietary Guidelines for Americans. Washington,USDA, December 2015.