Human Milk Oligosaccharides and the Mucosal Immune System
- Human milk oligosaccharides promo - te the mucosal immune protection through the microbiota and mucosal immune system.
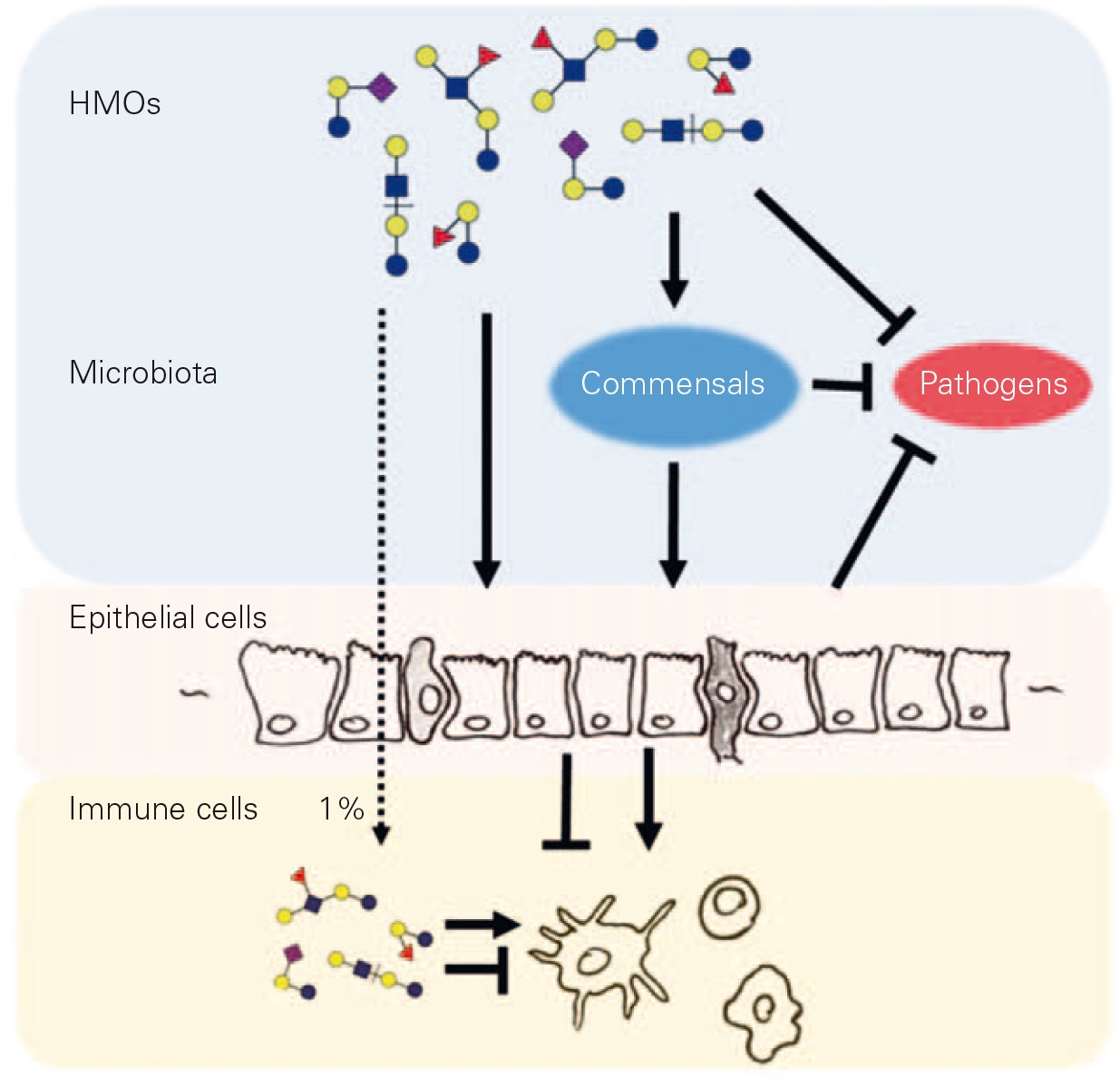
Breastmilk is the recommended and presumed evolutionary adapted nutrition for term-born healthy infants. Numerous meta-analyses showed that breastfeeding for longer periods results in decreased risks primarily for infections, but also for diabetes and overweight, while its effect on allergies is less clear [1]. Among the breastmilk components implicated in immune protection are human milk oligosaccharides (HMOs) [2]. HMOs are elongations of the milk sugar lactose with combinations of galactose, N-acetylglucosamine, fucose, and/or sialic acid. These elongations are structurally similar to glycans exposed on secreted mucins and cell surfaces in the form of glycolipids and glycoproteins. Cell surface glycans stabilize and modulate receptor functions commonly through the interaction with glycan- binding proteins and, due to their dominant, luminal exposure, are often primary docking sites for pathogens. The similarity of HMOs with mucin and cell surface glycans suggests that HMOs interfere with glycan-mediated processes that affect (i) the establishment of commensals, (ii) the adherence of pathogens, and (iii) mucosal cell reactivity (fi g. 1).
In the intestinal epithelium, enterocytes, enteroendocrine cells, and the chemosensory Tuft cells are candidate signal transducers to the mucosal immune cells. In model systems, HMOs stimulate enterocyte maturation and immune reactivity resulting in improved immune protection [3, 4]. Similarly, HMO exposure of immature human intestinal tissue shifts gene expression profi les towards immune maturation and reduced response to infl ammatory stimulation [5].
About 1% of ingested HMOs reach the systemic circulation and are excreted in urine, indicating that HMOs may also directly affect mucosal immune cells lying beyond the epithelial layer. Indeed, HMOs were shown to modulate proliferation, reactivity, and migration of isolated mononuclear cells, T cells, and dendritic cells [6–8].
For such effects, a strong HMO structure-function relation is often observed, meaning that not all HMOs or other oligosaccharides act in the same way. Taken together, an HMO-modulated intestinal environment including both the mucosal immune system and intestinal microbiota might explain at least partly the immune protection provided by prolonged breastfeeding and the proposed link between HMOs and reduced infectious diarrhea [9], lower respiratory tract infection and antibiotic use [10], and delayed onset of allergic eczema in C-section born infants [11].
- Victora CG, Bahl R, Barros AJ, et al: Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 2016;387:475–490.
- Hennet T, Borsig L: Breastfed at Tiffany’s. Trends Biochem Sci 2016;41:508–518.
- Kuntz S, Rudloff S, Kunz C: Oligosaccharides from human milk infl uence growth-related characteristics of intestinally transformed and non-transformed intestinal cells. Br J Nutr 2008;99:462–471.
- He Y, Liu S, Kling DE, et al: The human milk oligosaccharide 2’-fucosyllactose modulates CD14 expression in human enterocytes, thereby attenuating LPS-induced infl ammation. Gut 2016;65:33–46.
- He Y, Liu S, Leone S, Newburg DS: Human colostrum oligosaccharides modulate major immunologic pathways of immature human intestine. Mucosal Immunol 2014;7:1326– 1339.
- Amin MA, Ruth JH, Haas CS et al : H-2g, a glucose analog of blood group H antigen, mediates mononuclear cell recruitment via Src and phosphatidylinositol 3-kinase pathways. Arthritis Rheum 2008;58:689– 695.
- Comstock SS, Wang M, Hester SN, Li M, Donovan SM: Select human milk oligosaccharides directly modulate peripheral blood mononuclear cells isolated from 10-d-old pigs. Br J Nutr 2014;111:819–828.
- Kurakevich E, Hennet T, Hausmann M, Rogler G, Borsig L: Milk oligosaccharide sialyl(alpha2,3) lactose activates intestinal CD11c+ cells through TLR4. Proc Natl Acad Sci USA 2013;110:17444–17449.
- Newburg DS, Ruiz-Palacios GM, Morrow AL: Human milk glycans protect infants against enteric pathogens. Annu Rev Nutr 2005;25:37–58.
- Infant formula with human milk oligosaccharides supports age-appropriate growth and reduces likelihood of morbidity: A randomized controlled trial. G. Puccio, P. Alliet, C. Cajozzo, E. Janssens, G. Corsello, S. Wernimont, D. Egli, L. Gosoniu, N. Sprenger, P. Steenhout; Nutrition and Growth conference March 17–19, 2016, Vienna, Austria.
- Sprenger N, Odenwald H, Kukkonen AK, Kuitunen M, Savilahti E, Kunz C: FUT2-dependent breast milk oligosaccharides and allergy at 2 and 5 years of age in infants with high hereditary allergy risk. Eur J Nutr 2016, Epub ahead of print.
