How does the pandemic shape the future of allergies?
The COVID-19 pandemic posed numerous risks to everyone, but even more so for those with allergies, as those with poorly control asthma may be considered high-risk. With the interplay of various factors for inflammation, the susceptibility of an individual to the virus and management may be affected. In terms of the pandemic’s implications on allergies, measures taken against COVID-19 may have caused changes in the exposome, including air quality and circulation of respiratory viruses, but also in human microbiome. The repercussions of these measures on the incidence and severity of allergic diseases are currently under study. But telemedical services, as well as other strides towards better care and public health measures may help support the allergic individual better and create better outcomes in the future.
ABSTRACT
The COVID-19 pandemic posed an extraordinary challenge to societies and healthcare systems. Allergic individuals could not be an exception, being both directly and indirectly affected by the rapid and exponential spread of SARS-CoV-2. Although asthma was initially considered a risk factor for severe disease, evidence suggests that only poorly controlled asthmatics may constitute a high- risk group. A complex interplay between various factors involved in type 2 inflammation appears to determine an individual’s susceptibility to the virus and control of the infection. The impact of the pandemic on allergic patients’ mental health and trust in vaccines was also substantial, but through proper public health measures these effects are anticipated to abate. The implementation of innovative telemedical services was extensive and their use in everyday clinical practice will hopefully improve outcomes in various allergic diseases in the near future. Mitigation measures resulted in several changes in the exposome, including air quality and circulation of respiratory viruses, but also in human microbiome. The repercussions of these measures on the incidence and severity of allergic diseases are currently under study. Notwithstanding the detrimental consequences of SARS-CoV-2, the evolving pandemic offers the opportunity to investigate the long-term implications of various exposome changes; furthermore, it has provided opportunities towards improved care and public health measures to support the allergic individual.
INTRODUCTION
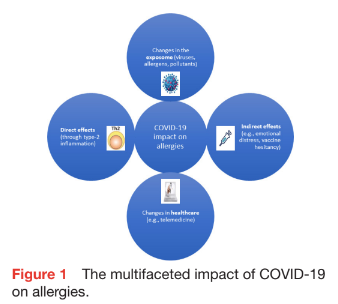
COVID-19 infection caused by SARS-CoV-2 has caused millions of deaths, substantial morbidity and an unprecedented worldwide response to alleviate its detrimental impact on individuals, community and healthcare services. It is estimated that 10%–40% of the population within different countries around the world suffer from at least one allergic disease, whereas the prevalence in developed countries reaches 20%.1 Therefore, it is pivotal to determine both short-term and long-term effects of the COVID-19 pandemic on allergic individuals and explore the complex interplay between physiological and social factors involved. Numerous studies and clinical observations have identified direct effects of SARS-CoV-2 on allergic individuals, associated with existing allergy-related pathophysiology. In addition, changes in healthcare organisation, as well as major changes in environmental exposures, have already had some impact and are expected to continue influencing susceptibility and expression of allergic diseases in the future (figure 1).
DIRECT EFFECTS OF SARS-COV-2 ON ALLERGIC INDIVIDUALS
It has been clearly shown that people with asthma are at increased risk of complications due to viral respiratory infections and viruses, most often rhinoviruses (RV), are the major triggers of acute asthma exacerbations.2 However, despite initial fears, it appears that allergic asthmatic individuals are not a high- risk group for adverse COVID-19 outcomes, with a possible exception when it comes to uncontrolled or severe asthma.3 In a large systematic review and meta-analysis including 5 87 280 patients with asthma, the risk of acquiring SARS-CoV-2 or hospital admission was in fact lower for asthmatics compared with controls.3 In school-aged children and adolescents, no association was observed between asthma and the risk of COVID-19 infection or severity.4–6 However, patients with severe asthma requiring high-dose inhaled corticosteroids (ICS) or oral corticosteroids had increased odds of hospital admission, but not intensive care unit (ICU) admission or mortality, whereas data on children are scarce.7 Importantly, patients with severe asthma treated with biologics, do not appear more likely to experience adverse outcomes due to COVID-19 infection, compared with the general population.8 Interestingly, there is also some evidence that anti-IL4R may be associated with improved outcomes.9
A protective effect of allergy on COVID-19 susceptibility and severity has been proposed and several mechanisms have been put forward to explain this.10 Type 2 inflammation has been associated with downregulation of membrane-bound ACE-2 in the airway epithelial cells, resulting in decreased viral uptake.10 11 Interleukin (IL)- 13, a potent mediator of type 2 response, can inhibit SARS-CoV2 infection of the bronchial epithelium.12 In contrast, several studies have shown that high levels of type 2 biomarkers were associated with worse COVID outcomes.13 It is possible that type 2 inflammation may have divergent effects on susceptibility to infection in comparison to inflammation control. Nevertheless, it appears that the net effect does not place allergic asthmatics in a high-risk group and it may even ‘protect’ them, provided their disease is well controlled.
A limited number of studies have explored the impact of COVID-19 on patients with allergic rhinitis. In a meta- analysis, no statistically significant difference was observed regarding the likelihood of severe infection or hospital admission between AR patients and controls.14
The COVID-19 pandemic has also affected patients with atopic dermatitis (AD). Current evidence is inconclusive on whether AD is linked with any changes in the risk of COVID-19 adverse outcomes.15 Of note, there is an evidence highlighting that patients with AD receiving dupilumab may have decreased odds of hospital admission or other adverse COVID-19-related outcomes, compared with patients on other treatments.16–18
The above effects, which will be certainly studied further, are likely to persist in the future, taking into account that SARS-CoV-2 has become endemic, and is still evolving.19 Potential ‘beneficial’ scenarios stemming from these findings, include increased adherence to medications, with improved outcomes, similar to the ones seen early in the pandemic6 and innovative management strategies. Reversely, if there is indeed a small protection against SARS-CoV-2 through T2 immunity, we should be vigilant to observe an increase in the incidence of allergies at the population level, particularly in young children.
INDIRECT EFFECTS OF COVID-19 ON ALLERGIC PATIENTS
Apart from the direct effects of COVID-19 on physical health, the recent pandemic caused increased emotional distress, affecting mental health.20 Allergic diseases are chronic conditions, which affect quality of life in varying degrees throughout their lifespan, and an association between them and psychiatric disorders has been documented.21 A survey-based study demonstrated increased risk of post-traumatic stress disorder and depression among allergic patients compared with adults without allergy,22 whereas another study noted increased psycho- social burden in adult patients with food allergy.23 In children, caregivers of patients with asthma or food allergy were disproportionally affected by the pandemic, reporting a higher psychological burden due to the perceived increased risk of severe disease from COVID-19 and the concern about limited access to emergency medical services.24 Hopefully, these effects will now be mitigated, and lessons learnt for improving healthcare services in this direction.
The pandemic triggered an unforeseen mobilisation of the scientific community, which resulted in the development and implementation of a mass vaccination programme in less than a year after the COVID-19 outbreak. While there is extensive evidence about vaccine safety, rare anaphylaxis events have been associated with vaccine administration,25 with polyethylene glycol in mRNA vaccines and polysorbate 80 (PS) were identified as the culprits for the immediate hypersensitivity reactions.26 Although the incidence of anaphylaxis is rare and revaccination of people with an immediate reaction to the first dose did not result in similar reactions in the vast majority of vaccine recipients,27 international allergy organisations issued clinical recommendations to ensure proper management of individuals at high risk for a reaction28 29 and to reduce vaccine hesitancy, especially in people with a history of allergy. Unfortunately, a considerable proportion of allergic individuals had lower levels of vaccine acceptance.30 This is an older and wider societal problem, which has been magnified by the pandemic. We do not expect to see major changes soon; conspiracy theories and low trust for administrations and media will continue, suggesting an important need for society-wide measures to regain trust and optimise public health!
Lastly, another aspect of the pandemic that is currently under investigation is long COVID and its implications. Although various hypotheses have been generated to explain a potential link between allergies and long COVID, there is insufficient evidence in the literature to establish any association.31
CHANGES IN HEALTHCARE ORGANISATION
In the last 15 years, various digital technologies have been developed and are increasingly investigated in clinical research to monitor symptoms and treatment adherence. The benefits of telemedicine had already been observed and a substantial number of patients had received some kind of remote services before the pandemic. However, the restrictions imposed at the beginning of the pandemic inevitably accelerated the adoption of several forms of telemedicine and resulted in a modified delivery of healthcare services across different patient populations.32 Face-to-face consultations were cancelled, immunotherapy sessions were postponed an oral food challenges could not be performed in a hospital environment. Consequently, allergists and clinical immunologists increased the number of virtual visits and the use of smart devices and apps to follow up their patients, which led to innovative modes of healthcare delivery at some institutions.33
A systematic review and meta-analysis has explored the effects of telemedicine on asthma control and quality of life in adult patients in the prepandemic era.34 The authors observed that combined telehealth approaches (telecase management and/or teleconsultation) improved symptom control, asthma outcomes and quality of life. In children, comparable asthma control was achieved between those receiving telemedical and usual care.35 The positive effects of remote consultation primarily concerned symptom burden, medication use and healthcare utilisation, whereas no effect was observed for pulmonary function. In addition, mixed results were reported regarding quality of life and patient satisfaction with the two different care modalities. After the pandemic outbreak, several studies examined the effectiveness of telemedicine and the resulting patient satisfaction. A retrospective study in a tertiary adult allergy centre in the first 2 months of the pandemic demonstrated that a significant proportion of new teleconsultations concerning both drug and non-drug-related reactions, did not require further allergy testing, high- lighting the existence of a subset of patients who could solely managed remotely.36 The vast majority of patients reported a good or very good experience with the new mode of allergy care.36 Interestingly, telemedicine was successfully used for both initiation and continuation of oral immunotherapy (OIT) during the pandemic.37 38
Nevertheless, the widespread adoption of new digital technologies in everyday clinical practice will require continuing satisfaction for both patients and providers. Patients cite that decreased waiting times, reduced transportation costs and easy accessibility as the main pros of telemedicine, whereas healthcare providers acknowledge that proper reimbursement, reliability and easy-to-use technology are the main drivers of their satisfaction.39 Undoubtedly, disparities regarding access to telemedical services are present on a worldwide scale, which may further negatively impact vulnerable groups.
Major advancements regarding both the extensive implementation of e-health modalities and the innovative testing of new potential digital tools were made during the pandemic. Most of these changes, however, took place under the pressure of the evolving pandemic and the extent that these expedited strategies will be translated into validated and sustained clinical practice, remains to be seen. In the era of personalised medicine, the advent of artificial intelligence and machine learning algorithms will pave the way for a radical transformation of allergy care. M-health applications, wearable sensors and home-based testing (eg, spirometry) will assist physicians to manage patients effectively, in a targeted and timely manner.40 There is an evidence indeed that the quality of m-health interventions in paediatric asthma improved during the pandemic.41 In conclusion, the rise of telemedicine in its various forms constituted a positive aspect of the unprecedented pandemic, offering continuous delivery of medical services to returning patients and increasing accessibility to new ones. Optimisation and standardisation of telehealth services is warranted so as to precisely assess the effect of each modality, alone or in combination, on patient important outcomes in various allergic diseases.
CHANGES IN THE EXPOSOME
Since the beginning of the pandemic, several non- pharmaceutical interventions were imposed for varying periods of time in order to limit the spread of SAR-CoV-2 infection at the individual and community level. These have also had a major impact on other respiratory pathogens, as well as allergens, pollutants, even access to food. The use of face masks in public places and public trans- port, intense hand hygiene and social distancing will most probably continue to some extent into the future. The initial strict mitigation strategies (eg, lockdown, border closing) resulted in an unprecedented global decrease in the incidence of common respiratory viruses and associated bacterial pathogens, such as Streptococcus pneumoniae.42 For most viruses, a sharp decline in their circulation was noted in the first months of the pandemic, which was followed by characteristic shifts in the seasonality of each virus across different parts of the world.42 Of note, the frequency of RV and respiratory enterovirus infections, after a short-lived decrease, remained relatively stable, despite the ongoing restrictive measures.43 It is possible that the presence of a viral protein capsid makes their viruses less susceptible to ethanol-containing disinfectants, compared with enveloped viruses (eg, influenza, respiratory syncytial virus). Moreover, some authors argue that viral interference may have contributed to this phenomenon.44 45 The gradual lifting of the various restrictive interventions was accompanied by the resurgence of viral infections, in some cases with higher intensity than before, highlighting the low population-based immunity.46 The microbial epidemiology and subsequent morbidity in the near future, is far from clear. The authors speculate that at the population level, morbidity may be ‘stabilised’ in the next year or 2. Nevertheless, effects on disease progress of individuals—once again mostly children—who have suffered from severe respiratory infections during this period, cannot be excluded. Close surveillance of the ‘COVID-19’ generation should be considered, as this ‘natural experiment’ is continuing. It is well established that colonisation of the gut at birth and in early life is crucial for immune system’s function and dysbiosis is a risk factor for allergen intolerance. Multiple factors implicated in allergy development were variably affected by the recent pandemic. COVID-19 infection during pregnancy resulted in increased rates of preterm births and caesarean sections,47 which in turn are established risk factors for atopy and other inflammatory diseases. The CORAL birth cohort study is an ongoing
project to examine the allergic and autoimmune dysregulation in infants born between March and May 2020, during the first SARS-CoV-2 lockdown in Ireland.48 The preliminary results demonstrate that although antibiotic use declined and breastfeeding rates increased at 12 months of observation compared with national prepandemic levels, the incidence of AD and egg sensitisation (but not egg allergy) rose. Interestingly, only 17% of the infants experienced any infective illness during the first year of life.
‘Stay-at-home’ orders were issued in most countries in the early phases of the pandemic. As a consequence, people spent more time indoors compared with the past, limiting their outdoors activities to a minimum. Apart from the detrimental effects on people’s physical and mental well-being in general, it is conceivable that patients allergic to house dust mite and other indoor allergens may experience worsening of their symptoms. This was shown by a study from China,49 a finding, however, that was not corroborated by any other studies. On the contrary, tree pollen sensitisation declined in school-aged children in Korea.50 Furthermore, the huge reduction in every kind of anthropogenic activities conferred a drop in air pollution.51 Several studies observed a statistically significant association between improved airway quality and reduced emergency room visits due to asthma.51 52 In addition, self-reported improvement of patients with AD was noted, possibly due to increased adherence and limited exposure to outdoor triggers.53 Finally, patients with food allergy were also affected by the pandemic in an unexpected way. A significant reduction in the rate of home epinephrine-treated reactions during the lockdown period compared with similar time periods in previous years and in the same year before and after the lockdown was observed in Israeli adults receiving OIT at home.54 The authors speculate that the avoidance of potential cofactors such as fatigue and exposure to viral infections, which may increase the likelihood or trigger reactions, has contributed to this phenomenon.
Finally, the use of face masks conferred an additional advantage to individuals with allergic rhinitis through reduction of patient-reported nasal and ocular symptoms.55 56 Face masks, therefore, could be used in high- risk environments with increased pollen concentration. The extensive use of hand sanitisers, especially in healthcare professionals, has led to increased occurrence of contact dermatitis and the large-scale utilisation of disinfectants may have long-term repercussions on the population health and the environment.57 58
CONCLUSION
Overall, respiratory infections are major triggers for asthma, food allergy, urticaria, drug allergy, etc. On the other hand, when infections are prevented, so is exposure to biodiversity, which is necessary for the development of a healthy immune response. In light of the changes in the circulation of respiratory viruses, the change in sensitisation patterns and the drop in air pollution in the last 2–3 years described above, prospective population- based studies and birth cohorts will elucidate the impact of these changes on the incidence and severity of allergic diseases in the future. However, we have confirmed that we can produce major impact on disease occurrence and frequency, through changes in exposure. We have also learnt that, as in the case of other interventions such as antibiotics, ‘blanket’ measures may have opposite medium-term results. Therefore, careful and balanced exposure control should receive much more attention and be explored. In the case for example, of face masks, use in high-risk settings, such as hospitals, or in the case of symptomatic individuals, should probably become a new paradigm for improved outcomes.
While many of the learnings from the COVID-19 pandemic may be useful for improving response times and efficacy in a potential similar event in the future, it is clear that pathogens and their characteristics may vary considerably. Transmission dynamics, infectivity and morbidity may differ, particularly in patients with allergy or asthma. Hence, the key learning and recommendation remains a coordinated, transparent and rapid international response, based on sound scientific principles.
The recent pandemic put forward a lot of challenges for allergic individuals, caregivers and practising allergists. This stressful period, however, may bear fruit. The unprecedented collaboration of the scientific community and the delivery of innovative medical services has already benefited millions of patients and this paradigm shift in some aspects of medical practice will hopefully translate into a more personalised and high-quality care for the majority of patients.
____________________________________________
Contributors. NP: manuscript writing and critical revision, MM: manuscript writing and critical revision. All authors approved the final version of the manuscript.
Funding. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests. None declared.
Patient consent for publication. Not applicable.
Provenance and peer review. Not commissioned; externally peer reviewed.
REFERENCES
Pawankar R. Allergic diseases and asthma: a global public health concern and a call to action. World Allergy Organ J 2014;7:12.
Oliver BGG, Robinson P, Peters M, et al. Viral infections and asthma: an inflammatory interface Eur Respir J 2014;44:1666–81.
Sunjaya AP, Allida SM, Di Tanna GL, et al. Asthma and risk of infection, hospitalization, ICU admission and mortality from COVID-19: systematic review and meta-analysis. J Asthma 2022;59:866–79.
Rao S, Hurst JH, Zhao C, et al. Asthma and the risk of SARS- CoV-2 infection among children and adolescents. Pediatrics 2022;149:e2021056164.
Mongkonsritragoon W, Prueksapraoprong C, Kewcharoen J, et al. Prevalence and risk associated with asthma in children hospitalized with SARS-CoV-2: a meta-analysis and systematic review. J Allergy Clin Immunol Pract 2022;10:1382–4.
Papadopoulos NG, Mathioudakis AG, Custovic A, et al. Childhood asthma outcomes during the COVID-19 pandemic: findings from the PeARL multi-national cohort. Allergy 2021;76:1765–75.
Lee B, Lewis G, Agyei-Manu E, et al. Risk of serious COVID-19 outcomes among adults and children with moderate-to-severe asthma: a systematic review and meta-analysis. Eur Respir Rev 2022;31:220066.
Papaioannou AI, Fouka E, Tzanakis N, et al. SARS-Cov-2 infection in severe asthma patients treated with biologics. J Allergy Clin Immunol Pract 2022;10:2588–95.
Sasson J, Donlan AN, Ma JZ, et al. Safety and efficacy of dupilumab for the treatment of hospitalized patients with moderate to severe Coronavirus disease 2019: A phase 2A trial. Open Forum Infect Dis 2022;9:ofac343.
Zhang H-P, Sun Y-L, Wang Y-F, et al. Recent developments in the immunopathology of COVID-19. Allergy 2023;78:369–88.
Jackson DJ, Busse WW, Bacharier LB, et al. Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2. J Allergy Clin Immunol 2020;146:203–6.
Bonser LR, Eckalbar WL, Rodriguez L, et al. The type 2 asthma mediator IL-13 inhibits severe acute respiratory syndrome Coronavirus 2 infection of bronchial epithelium. Am J Respir Cell Mol Biol 2022;66:391–401.
Sasson J, Moreau GB, Petri WA. The role of interleukin 13 And the type 2 immune pathway in COVID-19: a review. Ann Allergy Asthma Immunol 2023;130:727–32.
Xu C, Zhao H, Song Y, et al. The association between allergic rhinitis and COVID-19: a systematic review and meta-analysis. Int J Clin Pract 2022;2022:6510332.
Wu JJ, Martin A, Liu J, et al. The risk of COVID-19 infection in patients with atopic dermatitis: a retrospective cohort study. J Am Acad Dermatol 2022;86:243–5.
Musters AH, Broderick C, Prieto-Merino D, et al. The effects of systemic immunomodulatory treatments on COVID-19 outcomes in patients with atopic dermatitis: results from the global SECURE-AD registry. J Eur Acad Dermatol Venereol 2023;37:365–81.
Stingeni L, Hansel K, Antonelli E, et al. Atopic dermatitis in adolescents: effectiveness and safety of dupilumab in a 16-week real-life experience during the COVID-19 pandemic in Italy. Dermatol Ther 2021;34:e15035.
Ungar B, Glickman JW, Golant AK, et al. COVID-19 symptoms are attenuated in moderate-to-severe atopic dermatitis patients treated with dupilumab. J Allergy Clin Immunol Pract 2022;10:134–42.
Are EB, Song Y, Stockdale JE, et al. COVID-19 Endgame: from pandemic to Endemic? Vaccination, reopening and evolution in low- and high-vaccinated populations. J Theor Biol 2023;559:111368.
Kessler RC, Ruhm CJ, Puac-Polanco V, et al. Estimated prevalence of and factors associated with clinically significant anxiety and depression among US adults during the first year of the COVID-19 pandemic. JAMA Netw Open 2022;5:e2217223.
Tzeng N-S, Chang H-A, Chung C-H, et al. Increased risk of psychiatric disorders in allergic diseases: a nationwide, population- based, cohort study. Front Psychiatry 2018;9:133.
Gonzalez-Diaz SN, Martin B, Villarreal-Gonzalez RV, et al. Psychological impact of the COVID-19 pandemic on patients with allergic diseases. World Allergy Organ J 2021;14:100510.
Warren C, Sherr J, Sindher S, et al. The impact of COVID-19 on a national sample of US adults with food allergy. J Allergy Clin Immunol Pract 2022;10:2744–7.
Burrows AG, Ellis AK. Psychological impacts of Coronavirus disease 2019 on people with asthma, allergic rhinitis, and food allergy. Ann Allergy Asthma Immunol 2022;129:52–61.
Greenhawt M, Abrams EM, Shaker M, et al. The risk of allergic reaction to SARS-CoV-2 vaccines and recommended evaluation and management: a systematic review, meta-analysis, GRADE assessment, and international consensus approach. J Allergy Clin Immunol Pract 2021;9:3546–67.
Banerji A, Wickner PG, Saff R, et al. mRNA vaccines to prevent COVID-19 disease and reported allergic reactions: current evidence and suggested approach. J Allergy Clin Immunol Pract 2021;9:1423–37.
Chu DK, Abrams EM, Golden DBK, et al. Risk of second allergic reaction to SARS-Cov-2 vaccines: a systematic review and meta- analysis. JAMA Intern Med 2022;182:376–85.
Barbaud A, Garvey LH, Arcolaci A, et al. Allergies and COVID-19 vaccines: an ENDA/EAACI position paper. Allergy 2022;77:2292–312.
Turner PJ, Ansotegui IJ, Campbell DE, et al. COVID-19 vaccine- associated anaphylaxis: a statement of the world allergy organization anaphylaxis committee. World Allergy Organ J 2021;14:100517.
Batac ALR, Merrill KA, Askin N, et al. Vaccine confidence among those living with allergy during the COVID pandemic (ACCORD): a scoping review. J Allergy Clin Immunol Glob 2023;2:100079.
Warner JO, Warner JA, Munblit D. Hypotheses to explain the associations between asthma and the consequences of COVID-19 infection. Clin Exp Allergy 2022;52:7–9.
Papadopoulos NG, Custovic A, Deschildre A, et al. Impact of COVID-19 on pediatric asthma: practice adjustments and disease burden. J Allergy Clin Immunol Pract 2020;8:2592–9.
Alvaro-Lozano M, Sandoval-Ruballos M, Giovannini M, et al. Allergic patients during the COVID-19 pandemic-clinical practical considerations: an European Academy of allergy and clinical Immunology survey. Clin Transl Allergy 2022;12:e12097.
Chongmelaxme B, Lee S, Dhippayom T, et al. The effects of telemedicine on asthma control and patients' quality of life in adults: a systematic review and meta-analysis. J Allergy Clin Immunol Pract 2019;7:199–216.
Culmer N, Smith T, Stager C, et al. Telemedical asthma education and health care outcomes for school-age children: a systematic review. J Allergy Clin Immunol Pract 2020;8:1908–18.
Thomas I, Siew LQC, Rutkowski K. Synchronous telemedicine in allergy: lessons learned and transformation of care during the COVID-19 pandemic. J Allergy Clin Immunol Pract 2021;9:170–6.
Chua GT, Chan ES, Soller L, et al. Home-based peanut oral immunotherapy for low-risk peanut-allergic preschoolers during the COVID-19 pandemic and beyond. Front Allergy 2021;2:725165.
Maeta A, Takaoka Y, Nakano A, et al. Progress of home-based food allergy treatment during the Coronavirus disease pandemic in Japan: a cross-sectional multicenter survey. Children (Basel) 2021;8:919.
Nguyen M, Waller M, Pandya A, et al. A review of patient and provider satisfaction with telemedicine. Curr Allergy Asthma Rep 2020;20:72.
Ferrante G, Licari A, Fasola S, et al. Artificial intelligence in the diagnosis of pediatric allergic diseases. Pediatr Allergy Immunol 2021;32:405–13.
Dauletbaev N, Oftring ZS, Akik W, et al. A Scoping review of mHealth monitoring of pediatric bronchial asthma before and during COVID-19 pandemic. Paediatr Respir Rev 2022;43:67–77.
Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol 2023;21:195–210.
Kreger JE, Hershenson MB. Effects of COVID-19 and social distancing on Rhinovirus infections and asthma exacerbations. Viruses 2022;14:2340.
Dee K, Goldfarb DM, Haney J, et al. Human Rhinovirus infection blocks severe acute respiratory syndrome Coronavirus 2 replication within the respiratory epithelium: implications for COVID-19 epidemiology. J Infect Dis 2021;224:31–8.
Wu A, Mihaylova VT, Landry ML, et al. Interference between Rhinovirus and influenza A virus: a clinical data analysis and experimental infection study. Lancet Microbe 2020;1:e254–62.
Messacar K, Baker RE, Park SW, et al. Preparing for uncertainty: endemic paediatric viral illnesses after COVID-19 pandemic disruption. Lancet 2022;400:1663–5.
Metz TD, Clifton RG, Hughes BL, et al. Disease severity and perinatal outcomes of pregnant patients with Coronavirus disease 2019 (COVID-19). Obstet Gynecol 2021;137:571–80.
Hurley S, Franklin R, McCallion N, et al. Allergy-related outcomes at 12 months in the CORAL birth cohort of Irish children born during the first COVID 19 Lockdown. Pediatr Allergy Immunol 2022;33:e13766.
Liu Y, Yang S, Zeng Y, et al. Influence of the COVID-19 pandemic on the prevalence pattern of allergens. Int Arch Allergy Immunol 2023;184:43–53.
Song KB, Park MJ, Choi EJ, et al. Decreased pollen sensitization in school-age children after the COVID-19 pandemic: COCOA study. J Allergy Clin Immunol 2023;151:AB120.
Venter ZS, Aunan K, Chowdhury S, et al. Air pollution declines during COVID-19 lockdowns mitigate the global health burden. Environ Res 2021;192:110403.
Aix M-L, Petit P, Bicout DJ. Air pollution and health impacts during the COVID-19 lockdowns in Grenoble, France. Environ Pollut 2022;303:119134.
Chan Ng PPL, Kang AYH, Shen L, et al. Improved treatment adherence and allergic disease control during a COVID-19 pandemic lockdown. Pediatric Allergy Immunology 2022;33. 10.1111/pai.13688 Available: https://onlinelibrary.wiley.com/toc/13993038/33/1
Nachshon L, Goldberg MR, Levy MB, et al. Home epinephrine- treated reactions in food allergy oral immunotherapy: lessons
from the Coronavirus disease 2019 lockdown. Ann Allergy Asthma Immunol 2021;127:451–5.
Liccardi G, Bilo MB, Milanese M, et al. Face masks during COVID-19 pandemic lockdown and self-reported seasonal allergic rhinitis symptoms. Rhinology 2021;59:481–4.
Mengi E, Kara CO, Alptürk U, et al. The effect of face mask usage on the allergic rhinitis symptoms in patients with pollen allergy during the COVID-19 pandemic. Am J Otolaryngol 2022;43:103206.
Medina-Ramón M, Zock JP, Kogevinas M, et al. Asthma, chronic bronchitis, and exposure to irritant agents in occupational domestic cleaning: a nested case-control study. Occup Environ Med 2005;62:598–606.
Dhama K, Patel SK, Kumar R, et al. The role of disinfectants and sanitizers during COVID-19 pandemic: advantages and deleterious effects on humans and the environment. Environ Sci Pollut Res Int 2021;28:34211–28.

