NNIW91 - Nurturing a Healthy Generation of Children: Research Gaps and Opportunities
Infant and childhood nutrition form the basis of an individual’s health in later life. Multiple lines of evidence – from experimental to epidemiological –
Contents
- Foreword
- Early Development of Taste and Flavor Preferences and Consequences on Eating Behavior
Sophie Nicklaus, Camille Schwartz, Sandrine Monnery-Patris, and Sylvie Issanchou - Early Development of Food Preferences and Healthy Eating Habits in Infants and Young Children
Andrea Maier-Nöth - Effect of Parental Feeding Practices (i.e., Responsive Feeding) on Children’s Eating Behavior
Kimberley Mallan and Narissa Miller - Parental Feeding Practices and Associations with Children’s Food Acceptance and Picky Eating
Lisa R. Fries and Klazine van der Horst - What Children Eat in Developing Countries: Diet in the Etiology of Undernutrition?
Christiani Jeyakumar Henry - Children’s Eating Behaviors and Energy Intake: Overlapping Influences and Opportunities for Intervention
Ciarán G. Forde, Anna Fogel, and Keri McCrickerd - FITS and KNHS Overview: Methodological Challenges in Dietary Intake Data Collection among Infants, Toddlers, and Children in Selected Countries
Alison L. Eldridge - Kids Nutrition and Health Study in China
Dantong Wang - Feeding Patterns of Infants and Toddlers: The Mexico Case Study
Salvador Villalpando-Carrión and Alison L. Eldridge - The 2016 Feeding Infants and Toddlers Study: Dietary Intakes and Practices of Children in the United States from Birth to 48 Months
Regan Bailey, Shinyoung Jun, and Alison L. Eldridge - Usual Energy and Nutrient Intakes and Food Sources of Filipino Children Aged 6–12 Years from the 2013 National Nutrition Survey
Imelda Angeles-Agdeppa, Liya Dinney, and Mario V. Capanzana - Food and Nutrition in Malaysian Children
Norimah A. Karim and Nurliyana Abdul Razak - Breakfast: Shaping Guidelines from Food and Nutrient Patterns
Michael Gibney and Irina Uzhova - The Importance of Dietary Protein at Breakfast in Childhood
Leonidas Karagounis - Breakfast Consumption versus Breakfast Skipping: The Effect on Nutrient Intake, Weight, and Cognition
Carol E. O’Neil and Theresa A. Nicklas - Breakfast, Glycemic Index, and Cognitive Function in School Children: Evidence, Methods, and Mechanisms
Sandra I. Sünram-Lea - List of Speakers
Foreword
Infant and childhood nutrition is the basis of an individual’s health in later life. Multiple lines of evidence – from experimental to epidemiological – are converging to highlight the importance of this early period for metabolic programming, physiological growth, and cognition. This is the cornerstone of the “developmental origin of health and disease” (DOHAD) paradigm, underscoring the significance of infancy and early childhood for setting the foundation for health. Any public health intervention that seeks to improve the general health of a population or combat disease should, therefore, target infants and children in order to reap the greatest benefits. Yet, there is little mechanistic evidence to reveal how. Some of the answers can be found in studying diet and eating behavior: food choices and dietary habits go hand in hand with nutrition. Eating is a key skill that develops during early life. Between conception and childhood, the mode of feeding drastically evolves, from amniotic fluid, to breastfeeding, weaning, and independent feeding. Not only does the child learn how to eat, but also what to eat, how much, and in what context. During this time, infants discover the intrinsic properties of foods, along with the variety of tastes, flavors, and textures. These earliest sensations pave the way for food choice, steering an individual towards a lifetime of healthy (or unhealthy) eating patterns.
The 91st Nestlé Nutrition Institute Workshop on Nurturing a Healthy Generation of Children: Research Gaps and Opportunities, which took place in Manila (Philippines) in March 2018, highlighted the importance of childhood diets, eating behaviors, and potential impacts on development and health. The first session chaired by Prof. Sophie Nicklaus (University of Bourgogne-Franche Comté, France) examined the development of taste in infants, revealing how taste preferences are shaped in utero and throughout weaning, and guide the individual’s later food choices. The theme of the second session, led by Dr. Christiani Jeyakumar Henry (National University of Singapore), focused on what do children really eat in different parts of the world. FITS (Feeding Infants and Toddlers Study) and KNHS (Kids Nutrition and Health Study) provided a glimpse into the diets of children around the world, identifying nutrition gaps and potential areas for intervention. The workshop ended with a final session on the most important meal of the day: breakfast. This session chaired by Prof. Theresa A. Nicklas (Baylor College of Medicine, Houston, TX, USA) concluded the 3 days of the fascinating scientific forum.
The key learnings from this workshop provide valuable insight for policy makers, researchers, and health care professionals on how diet and feeding behavior during each of these stages can influence health and disease.
We would like to thank the three chairpersons Sophie Nicklaus, Christiani Jeyakumar Henry, and Theresa A. Nicklas for putting the scientific program together.
We would also like to thank all speakers and scientific experts in the audience who contributed to the workshop content and scientific discussions.
Finally, we thank Dr. Josephine Yuson-Sunga, her team in the Philippines, and the NNI team in Switzerland for their support and nice hospitality.
Natalia Wagemans, MD
Global Head
Nestlé Nutrition Institute
La Tour-de-Peilz, Switzerland
Early Development of Taste and Flavor Preferences and Consequences on Eating Behavior
Sophie Nicklaus, Camille Schwartz, Sandrine Monnery-Patris, and
Sylvie Issanchou
Early childhood is an important period for the development of health. Recent researches using different approaches (experimental and epidemiological) have shown the importance of this early period for metabolic programming. This general concept of “Developmental Origin of Health and Disease” (DOHAD) has been refined in humans to highlight the importance of the first 1,000 days for the development of the health status. Eating behavior also develops during this period, in particular because from conception until the age of 2 years, the mode of feeding drastically evolves, which involves that the child has to learn “how” to eat, but also what to eat, how much food to eat, and in which context. After birth, when foods are orally exposed, infants discover the intrinsic properties of foods, with a variety of tastes, flavors, textures, as well as energy densities. Here, we focus on deciphering the involvement of taste and olfaction in the early establishment of eating behavior. In the frame of the OPALINE French birth cohort (Observatory of Food Preferences in Infants and Children), taste and flavor preferences were studied in children in relation with food acceptance over the first 2 years of life.
At birth, previous works revealed evidence of differential preferences across tastes, with a preference for the sweet taste and a rejection of the bitter taste, and very few evidence of inborn flavor preference, except when infants had been previously exposed to flavors from the maternal diet. The later evolution of taste and flavor preferences has received little attention. Within the OPALINE cohort, we studied longitudinally in a group of 285 infants the evolution of taste preferences from 3 to 20 months [1] and the evolution of flavor preferences from 8 to 22 months [2]. Taste acceptance trajectories for all primary tastes and for a fat emulsion were modeled. For saltiness, acceptance increased sharply between the ages of 1 3 and 12 months. The trajectories of acceptance were parallel for sweetness, sourness, and the umami taste between 3 and 20 months, with sweetness being preferred. Between 12 and 20 months, the acceptance of all tastes, except bitterness, decreased, and at 20 months, only sweetness was not rejected. The acceptance of bitterness remained stable. For the fat emulsion, acceptance evolved from indifference to rejection. Between 8 and 22 months, unpleasant food odors (trimethylamine, dimethyl disulfide, and butyric acid) lead to avoidance behavior in infants, but pleasant food odors did not elicit specific behavior. Developmental changes were dependent on taste and flavor; thus, a general change in taste or flavor perception is unlikely.
Taste exposure (i.e., dietary exposure to a variety of foods) might partly explain the taste acceptance trajectories. We showed that a longer breastfeeding duration (likely associated to a longer exposure to the umami tasting glutamate found in breast milk) was associated to a higher preference for the umami taste at 6 months [3]. Moreover, simultaneous to the introduction to complementary foods, taste differential reactivity (within-subject variability across tastes) clearly increased. At the beginning of the complementary feeding period, we showed that a higher preference for sweet, sour, and umami tastes was associated to a higher acceptance of sweet-, sour-, and umami-tasting foods, respectively [4], and, similarly, that rejection of the odor of trimethylamine and of dimethyl disulfide were related to the rejection of fish and sulfurous cheeses, respectively [5]. Further in development, at 20 months, food neophobia was associated to flavor differential reactivity (withinsubject variability across flavors) but not to taste differential reactivity (within-subject variability across tastes) [6], underlining the importance of olfaction in the development of neophobic reactions. Further studies are necessary to establish a more complete understanding of the programming effect of early dietary taste and flavor exposure on later food choices.
References
- Schwartz C, Chabanet C, Szleper E, et al: Infant acceptance of primary tastes and fat emulsion: developmental changes and links with maternal and infant characteristics. Chem Senses 2017;42:593–603.
- Wagner S, Issanchou S, Chabanet C, et al: Infants’ hedonic responsiveness to food odours: a longitudinal study during and after weaning (8, 12 and 22 months). Flavour 2013;2:19.
- Schwartz C, Chabanet C, Laval C, et al: Breastfeeding duration: influence on taste acceptance over the first year of life. Br J Nutr 2013;109:1154–1161.
- Schwartz C, Chabanet C, Lange C, et al: The role of taste in food acceptance at the beginning of complementary feeding. Physiol Behav 2011;104:646–652.
- Wagner S, Issanchou S, Chabanet C, et al: Liking the odour, liking the food. Toddlers’ liking of strongly flavoured foods correlates with liking of their odour. Appetite 2014;81:60–66.
- Monnery-Patris S, Wagner S, Rigal N, et al: Smell differential reactivity, but not taste differential reactivity, is related to food neophobia in toddlers. Appetite 2015;95:303–309.
Early Development of Food Preferences and Healthy Eating Habits in Infants and Young Children
Andrea Maier-Nöth
Early development of taste and food pleasure plays an important role for children and has long-lasting influences on subsequent food preferences and choices. Eating a variety of foods is essential to achieve adequate coverage of macro- and micronutrients. However, children’s vegetable consumption often falls below current recommendations, highlighting the need to identify strategies that promote better acceptance of vegetables.
Apart from our innate liking for sweet foods and disliking for very bitter foods, sensory pleasure for foods is mostly acquired through our early eating experiences. Infants have a fine palate and more taste buds than adults when they are born. They have about 10,000 taste buds all around their tongue including the roof and the back and sides of their mouth. The flavors of what a mother eats while pregnant can reach the fetus and help set up flavor preferences later on. From birth, infants can taste and smell foods, an experience that can take place through human milk as the food eaten by the mother influences the flavor of her milk and, thereby, the child’s preference.
Thus, preferences for specific flavors develop early through milkrelated flavor exposure or even during pregnancy, allowing an easier acceptance of new flavors and textures. Breastfeeding favors the acquisition of a taste for a variety of foods. At weaning, food preferences develop due to repeated exposure to a variety of foods, especially vegetables and fruits. The persistence of these early influences seems to be long-lasting. Factors favoring the development of food acceptance at the beginning of complementary feeding include, in particular, the role of early variety, repeated exposure, timing of food introduction, and sensory properties (texture, taste, and flavors) (Fig. 1).
During the third year of life, most children enter a neophobic phase during which the introduction of new foods becomes difficult. However,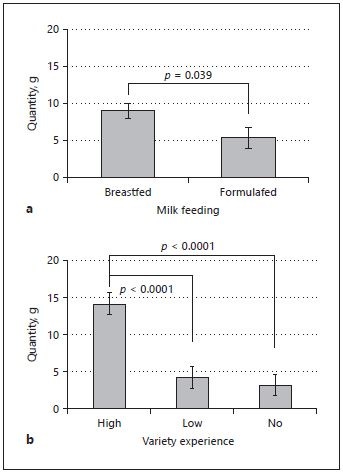
habits of eating a variety of vegetables and foods acquired early in weaning appear to attenuate this neophobia.
Recently, experimental studies have reported promising interventions that increase acceptance of vegetables and new foods. The first, offering infants a high variety of vegetables during weaning, increases acceptance of new foods, including vegetables. Frequent (daily) changes in vegetables offered appears to be more effective than changing every few days. In addition, breastfeeding (as opposed to formula feeding) followed by a wide variety of foods at weaning produces the greatest acceptance of new foods (Fig. 2). The second, offering an initially disliked vegetable at 8 subsequent meals, markedly increased acceptance for that vegetable.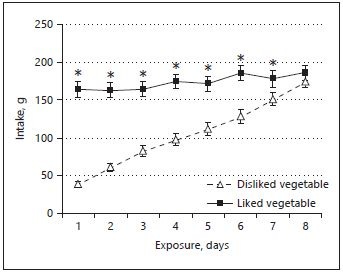
These effects have been shown to persist into childhood. This underlines the importance of promoting access to a variety of healthy foods (such as vegetables and fruits) in early childhood.
In conclusion, early experiences with vegetable variety during weaning can influence food choice and preference into childhood, and parents should actively encourage their children to try new vegetables and foods. If a new food is initially disliked, it is worth offering at 7–8 subsequent meals since this will usually lead to its long-lasting acceptance. These strategies provide the basis for science-based recommendations to help parents promote healthy eating habits in their children.
Suggested Reading
- Ahern SM, Caton SJ, Bouhlal S, Hausner H, Olsen A, Nicklaus S, Møller P, Hetherington MM: Eating a Rainbow. Introducing vegetables in the first years of life in 3 European countries. Appetite 2013;71:48–56.
- de Lauzon-Guillain B, Jones L, Oliveira A, Moschonis G, Betoko A, Lopes C, Moreira P, Manios Y, Papadopoulos NG, Emmett P, Charles MA: The influence of early feeding practices on fruit and vegetable intake among preschool children in 4 European birth cohorts. Am J Clin Nutr 2013;98:804–812.
- Jones L, Moschonis G, Oliveira A, De Lauzon-Guillain B, Manios Y, Xepapadaki P, Emmett P: The influence of early feeding practices on healthy diet variety score among pre-school children in four European birth cohorts. Public Health Nutr 2015;18: 1774–1784.
- Maier-Nöth AS: Gourmet oder Suppenkasper? Welche Faktoren beeinflussen das Ernährungsverhalten bei Kindern, und können wir es bereits früh in eine positive Richtung lenken? Pädiatrie & Pädologie 2017;52:280–283.
- Maier AS, Chabanet C, Schaal B, Leathwood PD, Issanchou SN: Breastfeeding and experience with variety early in weaning increase infants’ acceptance of new foods for up to two months. Clin Nutr 2008;27:849–857.
- Maier AS, Chabanet C, Schaal B, Issanchou S, Leathwood P: Effects of repeated exposure on acceptance of initially disliked vegetables in 7-month old infants. Food Quality and Preference 2007;18:1023–1032.
- Maier AS, Chabanet C, Schaal B, Leathwood P, Issanchou S: Food-related sensory experience from birth through weaning: Contrasted patterns in 2 nearby European regions. Appetite 2007;49:429–440.
- Nicklaus S: The role of food experiences during early childhood in food pleasure learning. Appetite 2016;104:3–9.
- Remy E, Issanchou S, Chabanet C, Nicklaus S: Repeated exposure of infants at complementary feeding to a vegetable puree increases acceptance as effectively as flavor-flavor learning and more effectively than flavor-nutrient learning. J Nutr 2013;143: 1194–1200.
Effect of Parental Feeding Practices (i.e., Responsive Feeding) on Children’s Eating Behavior
Kimberley Mallan and Narissa MillerHealthy eating habits formed in childhood track into later life [1]. Whilst some eating behaviors appear to have a genetic basis[2], the early feeding environment is considered critical to the development of healthy eating behaviors that will ensure children to effectively self-regulate energy intake through the ability to recognize and respond appropriately to internal cues of satiety and hunger, and ultimately achieve and maintain a healthy weight status [1, 3].
Parental feeding practices have been of interest to researchers and clinicians alike because they constitute modifiable risk factors for problematic child diet-related outcomes and appear to be amenable to intervention [3]. The purpose of this review is to examine current evidence for a causal relationship between feeding practices and child eating behaviors related to obesity risk.
Feeding practices are defined as content-specific, goal-directed strategies or behaviors used by parents in an attempt to control or modify their child’s diet and eating behaviors. DiSantis et al. [4] proposed that nonresponsive feeding practices that are controlling, coercive, or encourage children to eat for reasons other than hunger may interfere with a child’s ability to self-regulate their energy intake, i.e., to adjust their eating in response to internal feelings of fullness or satiety. It is proposed that when parents fail to recognize or respond appropriately to children’s internal cues of hunger or fullness, the child’s ability to self-regulate may be disrupted [4]. Therefore, the way in which feeding is responsive is an important element of the caregiver-child interaction.
Responsive feeding is defined as developmentally appropriate (not intrusive or controlling), prompt, and contingent responses to infant and child hunger and satiety. Also integral to responsive feeding are: establishing routines around mealtimes (eating at the same place and times), modeling appropriate behavior (making healthy choices), and ensuring children are seated [5].
Research in this field has predominantly focused on nonresponsive feeding practices including pressure to eat, instrumental, and emotional feeding (i.e., using food as a reward or to soothe the child), and restriction. In summary, current evidence generally suggests that nonresponsive feeding practices may be detrimental to the development of healthy eating behaviors in children. Pressure to eat appears to be associated with higher consumption of discretionary/snack foods but may be a practice that is used in response to child (low) weight concerns or food-avoidant eating behaviors such as food fussiness. Instrumental and emotional feeding have consistently been associated with emotional eating, food responsiveness, and higher snack food intake. Restricting children’s access to unhealthy snack foods appears to lead to greater interest in the restricted food and higher intake if the child is granted access in experimental settings. Finally, although a relatively new construct in the feeding literature, structure-related feeding practices appear to have protective effects on children’s eating behaviors.
Future research in this field that utilizes a longitudinal design assesses feeding practices and child eating concurrently, and attempts to ensure the validity of such measures is needed. Observational data that can complement self-report measures of both feeding practices and child eating behavior are one option for ensuring the validity of study findings. It is anticipated that greater understanding of the complex associations between these eating and feeding constructs can assist in improving our knowledge of the modifiable factors that contribute to the development of childhood obesity. These findings may be used in the design of future obesity prevention interventions targeting parental feeding practices.
References
- Savage JS, Fisher JO, Birch LL: Parental influence on eating behavior: conception to adolescence. J Law Med Ethics 2007;35:22–34.
- Llewellyn CH, Trzaskowski M, van Jaarsveld CH, et al: Satiety mechanisms in genetic risk of obesity. JAMA Pediatr 2014;168:338–344.
- Daniels LA, Mallan KM, Nicholson JM, et al: Outcomes of an early feeding practices intervention to prevent childhood obesity. Pediatrics 2013;132:e109–e118.
- DiSantis K, Hodges E, Johnson S, Fisher J: The role of responsive feeding in overweight during infancy and toddlerhood: a systematic review. Int J Obes (Lond) 2011;35:480–492.
- Black MM, Aboud FE: Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr 2011;141:490–494.
Parental Feeding Practices and Associations with Children’s Food Acceptance and Picky Eating
Lisa R. Fries and Klazine van der Horst
Many parents report that their children are picky eaters, with this behavior peaking at the age of 2–5 years. Some of the most common behaviors of picky eaters include limited dietary variety, neophobia, food refusals, less enjoyment of eating, and sensory sensitivities [Fries et al., unpubl. data], and this can be a source of stress for families during mealtimes.
Parents can influence their children’s mealtime behavior through the feeding practices they use when offering foods. This feeding relationship is a 2-way interaction, with children’s behaviors also affecting the parents’ feeding practices [1]. It is important to evaluate how parents can effectively intervene when encountering difficult eating behaviors in their children and to give them useful alternatives to parenting practices that have been shown to be counterproductive in establishing healthy eating habits.
Parents often give up after a food is refused a few times, but they should be encouraged to keep trying, as children may need to be exposed to a food several times before it is accepted. Different preparation methods change the taste, texture, and appearance of foods, and certain variants may be better accepted by children. Children can also become more familiar with food by cooking together with the caregiver [2] or even playing with food products.
Coercive feeding practices such as the use of pressure to eat should be avoided, as this can create negative associations with the food or meals, and could lead to more food refusals [3, 4]. Instead, one of the most successful ways to convince a child to try a food is for another person to model eating and enjoying it [5]. When families eat meals together and consume the same foods, this provides an excellent opportunity for modeling. Parents who give a reason why the child should taste something, such as by talking about the good taste of the food or its nutritional value, rather than simply telling them to eat it, may also help children be willing to taste a new food. This practice can also create intrinsic motivation for the child to eat the food in the future, as they will appreciate the food for its own properties (e.g., taste and health benefits), rather than only eating it when they expect an external reward.
Another practice to avoid is using one food as a reward for eating another food, as this can have negative short- [5] and long-term [6] consequences, such as food refusals and decreased liking of the target food. In contrast, non-food rewards, such as praise or stickers, can be used to encourage children to taste a food without creating these negative outcomes [7]. It should be noted that such rewards should be reserved for encouraging children to taste a food, but the child should not be required to finish the food. Using any kind of extrinsic rewards for plate cleaning can override children’s internal satiety cues and lead to eventual overeating.
It may be tempting for parents to prepare separate meals for picky eaters, but providing an alternative meal for a child who refuses the food initially offered reinforces the food refusal behavior. Further, if children are regularly provided with a limited range of “accepted” foods, this reduces opportunities for the child to experience new tastes or to have additional exposures to foods that they have not previously accepted. Thus, this behavior can perpetuate the child’s limited diet. As some children refuse foods as a way of expressing independence, parents may be able to avoid rejections by providing choices between 2 healthy options, as this allows children to express a preference without saying “no” altogether.
References
- Jansen PW, De Barse LM, Jaddoe VWV, et al: Bi-directional associations between child fussy eating and parents’ pressure to eat: who influences whom? Physiol Behav 2017;176:101–106.
- van der Horst K, Ferrage A, Rytz A: Involving children in meal preparation. Effects on food intake. Appetite 2014;79:18–24.
- Galloway AT, Fiorito LM, Francis LA, Birch LL: “Finish your soup”: counterproductive effects of pressuring children to eat on intake and affect. Appetite 2006;46:318–323.
- Fries LR, Martin N, van der Horst K: Parent-child mealtime interactions associated with toddlers’ refusals of novel and familiar foods. Physiol Behav 2017;176:93–100.
- Edelson LR, Mokdad C, Martin N: Prompts to eat novel and familiar fruits and vegetables in families with 1–3 year-old children: relationships with food acceptance and intake. Appetite 2016;99:138–148.
- Cooke LJ, Chambers LC, Añez EV, Wardle J: Facilitating or undermining? The effect of reward on food acceptance. A narrative review. Appetite 2011;57:493–497.
- Corsini N, Slater A, Harrison A, et al: Rewards can be used effectively with repeated exposure to increase liking of vegetables in 4–6-year-old children. Public Health Nutr 2013;16:942–951.
What Children Eat in Developing Countries: Diet in the Etiology of Undernutrition?
Christiani Jeyakumar Henry
It has been reported that nearly 50% of all deaths in children under 5 years may be attributed to undernutrition [1]. An understanding of what children eat is at the heart of our ability to prescribe an optimal diet for growth, development, and well-being. Undernutrition during the first 1,000 days of life has far-reaching consequences. It is a time when body tissues and brain development are forged, with long-term metabolic consequences. Stunting (short height for a child’s age), underweight (low body weight for age), and wasting (low weight for height) are the 3 commonly measured parameters of undernutrition. Around 25% of all children in low-/middle-income countries are permanently stunted in both their height and cognitive development. Stunting rates are up to 35% in Asia [2]. In fact, of the 34 countries where 90% of all the stunted children live, a significant number are in Asia. This statistic prompts us to reexamine the “the Asian enigma” to describe the lack of clarity on why the prevalence of childhood undernutrition and poor growth is much higher in this region than the rest of the world. An obvious starting point to explore this question is to examine critically what children eat in this region. There are surprisingly little reliable quantitative data on the energy intake in children living in many emerging economies. With increasing number of observational studies from around the world, some generalization can be made. The primary staples given to young children (in Asia and Africa) are largely composed of gruels made from rice, maize, cassava, yam, millet, and sago. These gruels are usually prepared by cooking these starches with water. During the process of cooking, the starch granules swell, gelatinize, and form thick, viscous pastes that are very low in energy density. Fed on such viscous foods, children are unable to consume sufficient feed to meet their energy and nutrient needs [3]. In an attempt to make such feeds acceptable to the infants, mothers may further tend to increase the water content of these porridges. This enables the porridge to be fed using a drinking cup. However, the further dilution of the porridge with water, although reducing the viscosity, drastically reduces the energy density of the feed. The first challenge in preparing foods with adequate nutrients for growth and maintenance in children is to construct and formulate foods with sufficient energy density, optimal viscosity, and mouthfeel. The opportunities and technical solutions that will enable us to develop foods of high nutrient value and energy for infant feeding will form the first part of this paper.
It is now well recognized that linear growth (height) is significantly influenced by the quality and quantity of protein intake along with the bioavailability of certain micronutrients, notably zinc and other trace elements. A major challenge facing infant feeding in Asia, Africa, and Latin America is the poor quality of protein consumed and the bioavailability of micronutrients. Novel strategies to improve protein quality and enhance bioavailability will be the focus of the final part of the paper. Despite nearly 8 decades of nutrition research on improving child nutrition, many children around the world have poor access to energy and nutrient-rich foods. Modern advances in agriculture, technology, and nutrition will enable us to develop a range of foods that will optimize growth, development, and human well-being.
References
- Black RE: Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–451.
- Bloem MW, de Pee S, Le Hop T, et al: Key strategies to further reduce stunting in Southeast Asia: lessons from the ASEAN countries workshop. Food Nutr Bull 2013;34(2 suppl 1):S8–S16.
- Kimmons JE, Dewey KG, Haque E, et al: Low nutrient intakes among infants in rural Bangladesh are attributable to low intake and micronutrient density of complementary foods. J Nutr 2005;135:444–451.
Children’s Eating Behaviors and Energy Intake: Overlapping Influences and Opportunities for Intervention
Ciarán G. Forde, Anna Fogel, and Keri McCrickerd
Early-life factors combine to influence the development of childhood overweight/obesity [1], yet the eating behaviors that support a sustained positive energy balance and unhealthy growth outcomes are less clear. The transition from “risk” to childhood obesity operates largely through the emergence of maladaptive eating behaviors that consolidate during childhood, remain stable, and predict sustained higher energy intakes and adiposity [2]. We examined associations between eating behaviors, energy intake, and body composition among children from the GUSTO cohort (Growing Up in Singapore towards Healthy Outcomes). Measures were collected at 2 time points (4.5 and 6 years) and included premeal portion selection, within-meal coding of oral processing behaviors, and postmeal measures of food responsiveness, which were examined alongside measured parental feeding practices and parent reports of their child’s appetitive traits.
Before lunch, children completed portion tasks on a computer, where they rated their appetite and then navigated through a series of food portion images to select their ideal portions of 8 familiar foods. Portions selected in the computer task significantly predicted the portions selected and consumed during a lunchtime meal. Children tended to pick more of foods they reported liking, but also smaller portions of foods they expected to be more filling, independently of whether they were liked. Importantly, the children who selected the largest portions tended to serve and consume a larger portion during the lunchtime meal.
At the 4.5- and 6-year time points, behavioral coding was used to capture each bite, chew, and swallow during the lunch, to subsequently derive a series of oral processing behaviors associated with energy intake (Fig. 1).
Children who ate at a faster rate (g/min) took larger bites, chewed less per bite, and consumed more energy at each meal (Fig. 2) [3, 4]. Faster
eating rates at 4.5 years predicted faster eating and higher energy intakes at 6 years, with the same oral processing behaviors driving eating rates at both time points. Children who ate faster at 4.5 years also had higher adiposity at 6 years, emphasizing a role for these behaviors in prospective weight gain. Portion selection and eating rate independently predicted higher energy intakes, but children who chose the largest portions, had the longest meals, and ate at the fastest rates consumed the most energy, highlighting an important overlap in behaviors that contribute to higher energy intakes.
Postmeal child responsivity to palatable food cues was assessed using the EAH paradigm (eating in the absence of hunger), where children were given free access to snacks after they had eaten to fullness. Children who demonstrated EAH consumed more energy cumulatively from lunch and the snack test [5]. This EAH behavior was consistent over time and linked to faster eating rates, highlighting an overlap between behaviors that contribute to higher energy intakes both within and outside the main meals.
Importantly, parents appear to be aware of their child’s appetitive traits, with faster eating and greater intake significantly correlated with higher “food responsiveness” and “enjoyment of food” reported by the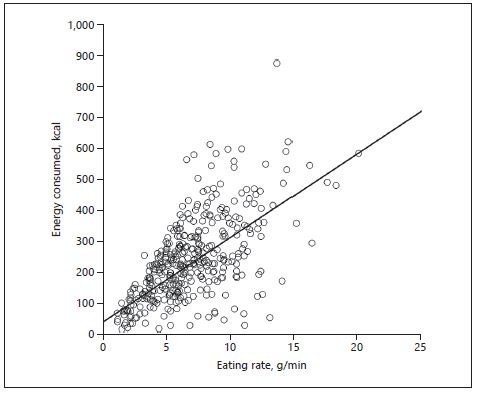
parents in the CEBQ (Child Eating Behavior Questionnaire) [6]. Some parents responded to their child’s behaviors during the meal by using feeding practices more frequently during the meal, particularly among girls. Despite this, children who were prompted more continued to eat quickly and consume more energy [7]. Our findings suggest a bidirectional relationship between parental feeding practices, child eating behaviors, and subsequent weight status.
Taken together, these findings highlight that higher energy intakes were consistently associated with a series of overlapping eating behaviors and parental feeding practices that were stable over time and most commonly found in children with highest BMIz scores. Our findings emphasize the need to go beyond targeting individual eating behaviors to consider the cumulative impact differences in energy selection, consumption, and associated parental feeding practices have on energy intake when developing interventions targeting children at risk of overweight or obesity.
References
- Aris IM, Bernard JY, Chen LW, et al: Modifiable risk factors in the first 1000 days for subsequent risk of childhood overweight in an Asian cohort: significance of parental overweight status. Int J Obes (Lond) 2018;42:44–51.
- Carnell S, Wardle J: Appetite and adiposity in children: evidence for a behavioral susceptibility theory of obesity. Am J Clin Nutr 2008;88:22–29.
- Fogel A, Goh AT, Fries LR, et al: A description of an “obesogenic” eating style that promotes higher energy intake and is associated with greater adiposity in 4.5-yearold children: results from the GUSTO cohort. Physiol Behav 2017;176:107–116.
- Fogel A, Goh AT, Fries LR, et al: Faster eating rates are associated with higher energy intakes during an ad libitum meal, higher BMI and greater adiposity among 4.5-yearold children: results from the Growing Up in Singapore Towards healthy Outcomes (GUSTO) cohort. Br J Nutr 2017;117:1042–1051.
- Fogel A, McCrickerd K, Fries LR, et al: Eating in the absence of hunger: stability over time and associations with eating behaviours and body composition in children. Physiol Behav 2018;192:82–89.
- Fogel A, Fries LR, McCrickerd K, et al: Oral processing behaviours that promote children’s energy intake are associated with parent-reported appetitive traits: results from the GUSTO cohort. Appetite 2018;126:8–15.
- Fogel A, Fries LR, McCrickerd K, et al: Prospective associations between parental feeding practices and children’s oral processing behaviours: results from the GUSTO cohort. Matern Child Nutr 2018, in press.
FITS and KNHS Overview: Methodological Challenges in Dietary Intake Data Collection among Infants, Toddlers, and Children in Selected Countries
Alison L. EldridgeFITS (the Feeding Infants and Toddlers Study) began in 2002 as a large-scale national telephone survey to study the eating patterns and nutrient intakes of infants and young children in the USA and was followed in 2008 by a second FITS. Both studies helped to fill a gap in knowledge and confirmed Nestlé’s commitment to understanding dietary patterns among children in these vulnerable age groups.
Building on the FITS model, Nestlé expanded their research program to include older children and launched the KNHS (Kids Nutrition and Health Study) in 2014. Together, FITS and KNHS investigate nutrient intakes, food groups consumed, food sources of nutrients, meal patterns, feeding practices, household demographic factors, and key behaviors related to energy intake and expenditure in infants and children in different countries around the world [1–5].
In each FITS and KNHS country, dietary intake was assessed using trained interviewers and multiple-pass 24-h recalls on 1 or more days (Table 1). The FITS and KNHS used data from national nutrition and health surveys when available. This was the case for KNHS in Australia, China, and the USA, and for FITS and KNHS in Mexico, the Philippines, and Russia. In China and the USA, the national surveys did not include infants or toddlers, so we collected data using similar methods (MING in China and FITS in the USA).
Although many countries with comprehensive national nutrition surveys use dietary recalls for individual-level intake estimations, other aspects of the survey methodology differed considerably. National surveys used in FITS and KNHS have collected data on intake at 1 day (Mexico), 2 nonconsecutive days (Australia, the Philippines, and the USA), or
Table 1. FITS and KNHS study countries, sources of data, participant characteristics, and dietary assessment methods used
| Study Name | Age | Participants,n | Dietary assessment method | |
| Australia | 2011-2012 National Nutrition and Physical Activity Survey (NNPAS) | 2 years and older | 2,213 (4-12 years) | Two 24-h recalls |
| China FITS | 2011-2012 Maternal Infant Nutrition Growth (MING) | Birth to 35 months | 1,409 (0-35 months) | One 24-h recall |
| China KNHS | 2011 China Health and Nutrition Survey (CHNS) | 2 years and older | 1,460 (4-13 years) | Three consecutive-day 24-h recalls |
| Mexico | 2012 Mexican National Health and Nutrition Survey (ENSANUT) | All ages | 2,057 (0-47 months) 3,985 (4-13 years) | One 24-h recall |
| The Philippines | 8th National Nutrition Survey 2013-2014 | All ages | 1,837 (0-35 months) 8,992 (3-12 years) | - |
| Russia | 2013 Russian National Nutrition Survey | All ages | 4,612 (0-47 months) 22,771 (4-13 years) | Two 24-h recalls, spring and fall |
| US FITS | 2016 Feeding Infants and Toddlers Study | Birth to 47 months | 3,235 (0-47 months) | Two 24-h recalls |
| US KNHS | 2009-2012 National Health and Nutrition Examination Survey | 2 years and older | 3,647 (4-13 years) | Two 24-h recalls |
3 consecutive days of intake (China). In Russia, 2 days of intake data were collected, 1 in spring and 1 in autumn. Food composition tables varied by country, both in number of nutrients and completeness of the databases. Different countries used different age classifications and different food grouping schemes. Not all surveys recorded details about the meals or times when foods were consumed.
To address these issues, a common analysis approach has been applied across all FITS and KNHS countries. The standard analysis evaluates nutrient intakes by looking at means and distributions of intakes, and compares them with established dietary reference intakes. We evaluate meal patterns, including the percent consuming and skipping different meals and snacks and timing of consumption. Food groups are applied to all foods and beverages reported, and these are used to look at eating patterns, including the complementary feeding transition, and to understand the top sources of energy and nutrients in the diet.
As much as possible, the FITS and KNHS have standardized reporting of age categories (typically 0–5.9, 6–11.9, 12–23.9, and 24–47.9 months, and 4–8 and 9–13 years of age) and food grouping systems so comparisons could be made. Aligning food groups is challenging as the specificity needed for some food groups differs depending on the country. We have supported work to impute nutrient values to complete datasets for nutrients of interest when needed (e.g., total sugar in Mexico and China; fiber, sodium, and total sugar in the Philippines).
In summary, the FITS and KNHS are part of a global Nestlé research initiative to study dietary intakes and related behaviors in infants, toddlers, and children. We have evaluated national survey data where they exist, and when not available, we have conducted our own studies to fill the gaps in knowledge. To address methodological issues, we implemented a common analysis approach, supported work to impute nutrient values to complete food composition databases, and harmonized food grouping systems so comparisons could be made across countries. This overview is accompanied by case studies sharing results from countries that comprise the current FITS and KNHS.
References
- Bailey RL, Catellier D, Jun S, et al: Total usual nutrient intakes of U.S. Children (<48 months): findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr 2018;148:1557S–1566S.
- Denney L, Afeiche MC, Eldridge AL, Villalpando-Carrión S: Food sources of energy and nutrients in infants, toddlers, and young children from the Mexican National Health and Nutrition Survey 2012. Nutrients 2017;9:494.
- Fayet-Moore F, Peters V, MConnel Al, et al: Weekday snacking prevalence, frequency, and energy contribution have increased while foods consumed during snacking have shifted among Australian children and adolescents: 1995, 2007 and 2011–12 National Nutrition Surveys. Nutr J 2017;16:65.
- Martinchik AN, Baturin АК, Keshabyants EE, et al: Dietary intake analysis of Russian children 3–19 years old (in Russian). Voprosy Pitaniia (Problems Nutr) 2017;86:50–60.
- Wang H, Wang D, Ouyang Y, et al: Do Chinese children get enough micronutrients? Nutrients 2017;9:397.
Kids Nutrition and Health Study in China
Dantong Wang
KNHS (the Kids Nutrition and Health Study) is a global research project focusing on the assessment of children’s dietary intakes and eating behaviors, including nutrient intakes, food patterns, and physical activities. China is one of the countries involved in the study. KNHS China is a collaboration between the China National Institute of Nutrition and Health (NINH; Beijing, China), the University of North Carolina (UNC; Chapel Hill, NC, USA), and the Nestlé Research Center (NRC; Lausanne, Switzerland). Data used in this study were from the 2011 China Health and Nutrition Survey (CHNS).
In the 2011 CHNS, a multistage randomized cluster sampling method was used to recruit participants from 9 provinces and 3 mega cities (Beijing, Shanghai, and Chongqing) representing different geographies and economic development stages, with communities from both urban and rural areas. The KNHS China project focused on children 4–13 years old. In total, dietary intake data from 1,481 children in the age range were analyzed. In some publications, the age range was extended from 4–13 to 4–17 years (1,905 subjects) to provide information on a broader age spectrum. Individual dietary data were collected using 24-h recalls on 3 consecutive days (2 weekdays and 1 weekend day). For children younger than 12 years, the mother or a caregiver who handled food preparation and feeding in the household was interviewed. The interviews were conducted by trained field interviewers with the assistance of food models and pictures. Household edible oils, sugar, and salt consumption were determined on a daily basis by calculating the changes in the home food inventory by weighing [1]. Food recalls were coded and analyzed to calculate nutrient intakes using the Chinese Food Composition Tables published in 2009 [2].
We found that, compared to dietary intake recommendations, Chinese children had low intakes of micronutrients such as calcium and vitamin D. The intake of dietary fiber was low in 97% of children, whereas the intakes of saturated fat and sodium were excessive in 57 and 85% of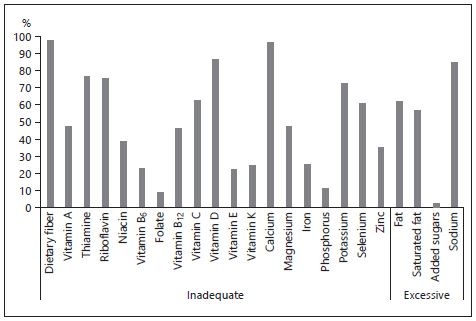
children, respectively (Fig. 1). Geographic location and socioeconomic status have an impact on food quality and nutrient intakes. Children from urban areas and from higher-income households were more likely to have higher micronutrient intakes and consume more animal source foods, especially dairy products, than those from rural areas and from lower-income households [3]. We observed the double burden of malnutrition in Chinese children: the prevalence of overweight or obesity in children was higher in urban areas and higher-income families than in rural settings and those from lower-income households [4]. The disparity found in this study suggests that specific strategies are needed to improve diet quality and address nutrient shortfalls in different community types.
We also reported that almost all children had 3 main meals, breakfast, lunch, and dinner, and over 70% of them reported having snacks, which contributed 10% of total daily energy. Children 9–13 years old consumed more salty snacks and less fruits and dairy products than children 4–8 years old did, which deserves attention [5]. Promoting healthy food choices in snacking could contribute to the improvement in nutritional quality of the total diet.
In conclusion, the KNHS China results suggest that a comprehensive approach that includes nutrition education, nutrition intervention programs targeting vulnerable populations, and promotion of physical activity inside and outside of school is needed to improve the nutrition and health status of Chinese children.
References
- Zhang B, Zhai FY, Du SF, Popkin BM: The China Health and Nutrition Survey, 1989– 2011. Obes Rev 2014;15(suppl 1):2–7.
- Chinese Nutrition Society: Chinese Dietary Reference Intakes (Edition 2013) (in Chinese). Beijing, Science Press, 2014.
- Zhang J, Wang D, Eldridge AL, et al: Urban-rural disparities in energy intake and contribution of fat and animal source foods in Chinese children aged 4–17 years. Nutrients 2017;9:526.
- Piernas C, Wang D, Du S, et al: The double burden of under- and overnutrition and nutrient adequacy among Chinese preschool and school-aged children in 2009–2011. Eur J Clin Nutr 2015;69:1323–1329.
- Wang D, van der Horst K, Jacquier EF, et al: Snacking patterns in children: a comparison between Australia, China, Mexico, and the US. Nutrients 2018;10:198.
Feeding Patterns of Infants and Toddlers: The Mexico Case Study
Salvador Villalpando-Carrión and Alison L. EldridgeUnderstanding the feeding patterns of Mexican infants and toddlers has required a large amount of effort due to the lack of recent reliable data. The double burden of obesity and micronutrient deficiency has caused alarm, identifying the need to discover when and how inadequate consumption of nutrients take place in such a diverse country. The types of foods and beverages that children consume have drastically changed in recent years, although there is poor factual knowledge around this matter. Another issue is that many physicians and health care professionals are bystanders in the practice of complementary feeding. There is a national recommendation for the introduction of complementary feeding that serves as a nationwide reference. Breastfeeding is strongly recommended. The national policy is for exclusive breastfeeding for at least 6 months, and introduction of complementary foods should not start before this age.
FITS Mexico (the Feeding Infants and Toddlers Study) was initiated to address the lack of knowledge of the actual feeding patterns of Mexican children. Secondary data analyses from a nationally representative sample of over 5,000 children from ENSANUT 2012 (Encuesta Nacional de Salud y Nutrición – the Mexican National Health and Nutrition Survey) were used to review the feeding and drinking patterns of Mexican children in depth [1–4]. Micronutrient and food sources of nutrients were analyzed. Appropriate and inappropriate foods and beverages were considered at the end point analyses of the feeding patterns. Also, a broad country panel of experts were involved in developing new feeding recommendations according to the FITS findings for healthy infants [5].
Low rates of exclusive breastfeeding were found in infants less than 6 months old [1]. We also reported that 31 and 35% of 6- to 11.9-monthold infants consumed cow’s milk or sugar-sweetened beverages, respectively [2]. Few infants received iron-rich food sources, such as fortified infant cereal or meats. One half of 6- to 47.9-month-old children consumed fruit, but 85% did not consumed vegetables as a distinct serving on the day of the recall. After 12 months of age, over 80% of toddlers consumed some type of sweet or sugar-sweetened beverages on any given day. Between 18 and 36% of toddlers did not meet the estimated average requirement for iron, and about 40% did not meet that for zinc. In contrast, more than 30% of toddlers exceeded the tolerable upper intake level of sodium daily [3].
Feeding patterns in Mexican children seem to be established early in life. Food groups consumed with poor micronutrient intakes and high energy consumption might explain the nutritional condition for the Mexican population through all age groups. Regional experts have used this information to set new and more strict recommendations for child feeding [5]. Public policy must change accordingly. Continuous study of feeding patterns in a population, especially in children, will be a powerful tool to monitor health and nutrition status for the whole country.
References
- Deming D, Reidy K, Afeich M, et al: Early feeding patterns among Mexican babies: findings from the National Health and Nutrition Survey 2012 and implications for health and obesity prevention. BMC Nutr 2015;1:40.
- Afeiche MC, Villalpando-Carrion S, Reidy KC, et al: Many infants and young children are not compliant with Mexican and international complementary feeding recommendations for milk and other beverages. Nutrients 2018;10:E466.
- Piernas C, Miles D, Deming D, et al: Estimating usual intakes mainly affects the micronutrient distribution among infants, toddlers and pre-schoolers from the 2012 Mexican National Health and Nutrition Survey. Public Health Nutr 2016;19:1017–1026.
- Denney L, Afeiche M, Eldridge A, Villalpando-Carrion S: Food sources of energy and nutrients in infants, toddlers, and young children from the Mexican National Health and Nutrition Survey 2012. Nutrients 2017;9:E494.
- Romero-Velarde E, Villalpando-Carrion S, Perez-Lizaur AB, et al: Consenso para las prácticas de alimentación complementaria en lactantes sanos. Bol Med Hosp Infant Mex 2016;73:338–356.
The 2016 Feeding Infants and Toddlers Study: Dietary Intakes and Practices of Children in the United States from Birth to 48 Months
Regan Bailey, Shinyoung Jun, and Alison L. EldridgeThe Feeding Infants and Toddlers Study (FITS) is a periodic national cross-sectional survey to examine the diets and feeding practices of US infants and children, with ages categorized to represent important transition times in the diet: younger infants (birth to 5.9 months), older infants (6–11.9 months), toddlers (12–23.9 months), younger preschoolers (24–36.9 months), and older preschoolers (36–47.9 months). FITS 2016 collected dietary data using a 24-h dietary recall (n = 3,235), with a replicate in a representative subsample (n = 799) [1, 2]. Energy, nutrient intakes, and compliance with dietary reference intakes were estimated using the National Cancer Institute method. Infant feeding practices and food group consumption were also assessed by participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) that provides food packages to US children <5 years.
Infant Feeding Practices (Birth to 12 Months). Initiation and duration of breastfeeding were higher in 2016 compared to previous FITS surveys but remained below public health recommendations. Exclusive breastfeeding varied by race/ethnicity with non-Hispanic White (40%) and Hispanic (36%) (birth to 3.9 months) having significantly higher rates than non-Hispanic Black infants (20%). Transition to complementary foods tended to occur earlier in formula-fed than breastfed infants.
Energy and Nutrients. Energy intakes and dietary diversity increased with age; however, vitamins D and E were low in all age groups. Nutrient intakes of the younger infants were largely adequate except for iron among older infants, with 18% of those 6–11.9 months below the estimated average requirement. After 12 months, few exceed the adequate intake for fiber and potassium: 3 and 3% among toddlers; 9 and 6% among younger preschoolers; and 8 and 4% among older preschoolers, respectively. Concerns exist about excessive intakes of retinol and zinc with estimates ranging from 32 to 49% for retinol and from 41 to 69% for zinc above the upper intake level. Among preschoolers, more than 70% exceeded the upper intake level for sodium and >60% exceeded the saturated fat recommendations.
Foods and Beverages. These nutrient imbalances noted in FITS 2016 are likely the result from lower-than-recommended intakes of vegetables and whole grain foods and higher-than-recommended intakes of sugar-sweetened beverages and savory snacks. Iron-rich infant cereal was consumed by about one-half of those 4–12 months old. Close to 20% of toddlers and preschoolers did not consume cow’s milk, an excellent source of vitamin D and calcium, while all in this age group consumed grains; 40% did not consume whole grains. Fruit consumption was adequate across all groups, but vegetable intakes were lower and comprised primarily fried potatoes. After 12 months, all children exceeded energy recommendations from added sugars, primarily coming from sweet bakery foods, sugar-sweetened beverages, and candy. High sodium intakes were associated with processed meats and savory snacks.
Women, Infants, and Children. WIC reaches 51% of US infants and about 30% of children 1–5 years. WIC eligibility is based on income; foods provided are tailored to meet age-specific nutrient needs. WIC infants were less likely to be breastfed than higher-income children; however, mean micronutrient intakes were higher for WIC infants possibly due to consumption of fortified infant formula. WIC preschoolers had a lower risk of inadequate vitamin D than income-eligible nonparticipants. High intakes of sodium, added sugars, and sweetened beverages were especially of concern among WIC participants [3].
Conclusion. The dietary intakes of US infants (<12 months) were nutritionally adequate, with exceptions noted for iron (6–11.9 months). However, starting at 12 months, we observed higher-than-recommended intakes of sodium, added sugars, saturated fat, retinol, and zinc combined with low intakes of potassium, fiber, vitamin D, and vitamin E. Shifting dietary patterns to enhance whole grains, fruit, vegetables, and low-fat dairy while limiting processed meats, sources of added sugars, and savory snacks would help align nutrient intakes with guidelines.
References
- Anater AS, Catellier DJ, Levine BA, et al: The Feeding Infants and Toddlers Study (FITS) 2016: study design and methods. J Nutr 2018;148:1516S–1524S.
- Bailey RL, Catellier DJ, Jun S, et al: Total usual nutrient intakes of US children (under 48 months): findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr 2018;148:1557S–1566S.
- Jun S, Catellier DJ, Eldridge AL, et al: Usual nutrient intakes from the diets of US children by WIC participation and income: findings from the Feeding Infants and Toddlers Study (FITS) 2016. J Nutr 2018;148:1567S–1574S.
Usual Energy and Nutrient Intakes and Food Sources of Filipino Children Aged 6–12 Years from the 2013 National Nutrition Survey
Imelda Angeles-Agdeppa, Liya Dinney, and Mario V. CapanzanaIt is important to assess the food intake of children aged 6–12 years in order to possibly link this with other nutrition-specific interventions to address malnutrition [1]. This study evaluated usual energy and nutrient intakes and food sources of school-age children in the Philippines. Data were from the 2013 National Nutrition Survey. A total of 6,565 children 6–12 years old from all sampled 8,592 households were interviewed for first-day 24-h dietary recall. A second-day recall was obtained from a random subsample (50% of the children). Usual energy and nutrient intakes were estimated using the PC-SIDE program [2]. Energy inadequacy was compared with estimated energy requirements considering active physical activity. Macronutrients were evaluated using the acceptable macronutrient distribution ranges. Micronutrient inadequacy was computed using the estimated average requirements (EAR) cutoff point method [3].
Results showed that mean energy intake (1,358 kcal) of all children was 24.6% below the estimated energy requirements. Forty-two percent had total fat intake as percentage of total energy below the lower range of acceptable macronutrient distribution ranges (AMDR), and hence most of the energy was provided by carbohydrates (Table 1). About 16% of children had protein intake below the EAR [4]. The mean intakes of total sugar and dietary fiber were 26.8 and 6.9 g/day, respectively (Table 1).
The prevalence of inadequate total fat intake as percent energy intake was especially high in rural areas (60%). In children from the poorest quintile, a higher proportion did not meet the AMDR for total fat (80%), while 14% of the children from the richest quintile exceeded the AMDR. Furthermore, 36% of children from the poorest quintile exceeded the AMDR for carbohydrates (Table 1).
The vitamin with the highest prevalence of inadequacy was vitamin C (81%). Nutrient inadequacy for other vitamins was: folate (70%),
Table 1. Mean usual nutrient intake and intake distribution for all children 6–12 years old (n = 6,565)
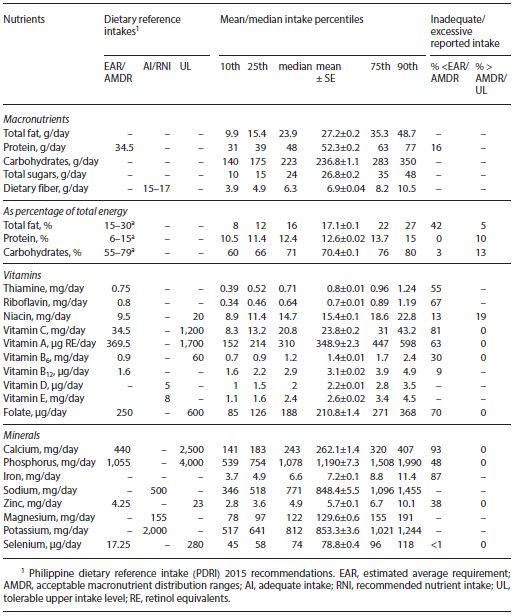
riboflavin (67%), and vitamin A (63%), vitamin B6 (30%), niacin (13%), and vitamin B12 (9%). The average intakes of vitamins D and E were 2.2 µg/day and 2.6 mg/day, respectively, and these were very low compared with the recommendations [4]. A high prevalence of inadequacy was also observed for calcium (93%), iron (87%), phosphorus (48%), and zinc
Table 2. Percentage contributions of the top 10 food groups to selected macro- and micronutrient intakes among Filipino school-age children
(38%). Usual intake of sodium, magnesium, and potassium were 848, 130, and 853 mg/day, respectively. The mean intake of sodium exceeded the requirement, while the intake of potassium and magnesium were below the requirement (Table 1).
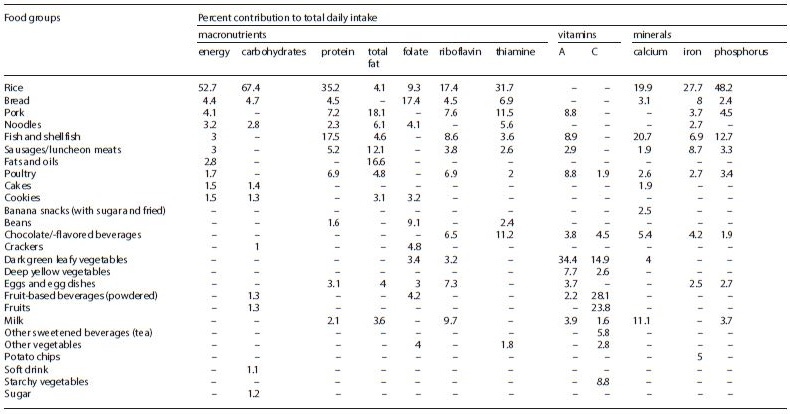
Refined rice is the major source of energy, carbohydrates, and protein providing 53, 67, and 35% of total intake, respectively (Table 2). Rice also contributed a large amount of phosphorous (48%), iron (28%), calcium (20%), thiamine (32%), and riboflavin (17%). Another major contributor of calcium intake was fish and shellfish (21%). The major sources of fats are pork, sausages, and oils. The major source of vitamin C is fortified fruit-based drinks. Dark green leafy vegetables were the major source of vitamin A (34%). Bread was a major source of folate, contributing 17% (Table 2).
Applying usual intake analysis in Filipino children, this study demonstrated that the intakes of fat and many micronutrients were markedly inadequate as evidenced by a high prevalence of inadequate intakes of fat and most vitamins and minerals. The shortfalls in nutrients can be largely explained by the high intake of refined rice, which is the major source of many key nutrients, while nutrient-dense foods such as milk, fruits, and vegetables played little role in the diet. The results are informative to nutrition policy and education both for parents and health care professionals, and could be used for the development of various public health strategies to improve diet quality and address nutrient shortfalls in the diets of this population.
References
- International Food Policy Research Initiative: Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030. Washington, International Food Policy Research Institute, 2016, http://www.ifpri.org/publication/ global-nutrition-report-2016-promise-impact-ending-malnutrition-2030.
- Nusser SM, Carriquiry AL, Dodd KW, Fuller WA: A semi-parametric transformation approach to estimating usual daily intake distributions. J Am Stat Assoc 1996;91:1440–1449.
- Lopez-Olmedo N, Carriquiry AL, Rodriguez-Ramirez S, et al: Usual intake of added sugars and saturated fats is high while dietary fiber is low in the Mexican population. J Nutr 2016;146:1856S–1865S.
- Food and Nutrition Research Institute–Department of Science and Technology (FNRI–DOST): Philippine Dietary Reference Intakes (PDRI) 2015. Taguig City, FNRI–DOST, 2015.
Food and Nutrition in Malaysian Children
Norimah A. Karim and Nurliyana Abdul RazakRapid socioeconomic growth has led to nutrition and health transition in Malaysia. Childhood obesity has become a major concern. The findings from 2 nationwide studies, namely, SEANUTS Malaysia (the South East Asian Nutrition Survey of Malaysian Children) [1] and the MyBreakfast study [2] showed that between 13 and 17% of school children aged between 6 and 12 years were either overweight or obese, with similar prevalence in both urban and rural areas. These studies showed that overweight and obesity problems among Malaysian children should be of concern, as 3 in 10 children are either overweight or obese, irrespective of the areas where they reside.
Table 1 shows the prevalence of children not achieving the recommended nutrient intake (RNI) for selected macro- and micronutrients. The mean energy intake of the children ranged from 1,800 to 1,900 kcal/ day. The majority of the children in both studies (SEANUTS Malaysia [1] and MyBreakfast study [2]) achieved the Malaysian RNI for energy and protein; however, at least two-thirds of the children did not achieve the RNI for calcium. About 9 in 10 children did meet the RNI for vitamin D in the MyBreakfast study [2]. These findings are worrying as both calcium and vitamin D are important nutrients for bone health. In the MyBreakfast study, breakfast was defined as the first eating occasion after an overnight sleep until 10 a.m. on weekdays and 11 a.m. on weekend days [2].
In the MyBreakfast study, the prevalence of breakfast skippers (ate breakfast 0–2 days/week) and irregular breakfast eaters (ate breakfast 3–4 days/week) was 9.3 and 10.8%, respectively, while 79.9% were found to be regular breakfast eaters (ate breakfast 5–7 days/ week) [2]. In the SEANUTS Malaysia, breakfast was defined as the first eating occasion consumed by the children before 10 a.m., and irregular breakfast eaters were defined as children who skipped breakfast on a daily basis [3]. Table 2 shows the distribution of breakfast consumption among primary school children in the SEANUTS Malaysia and the MyBreakfast study.
Table 1. Prevalence of Malaysian primary school children (6–7 to 12 years) not achieving the RNI of selected macronutrients and micronutrients
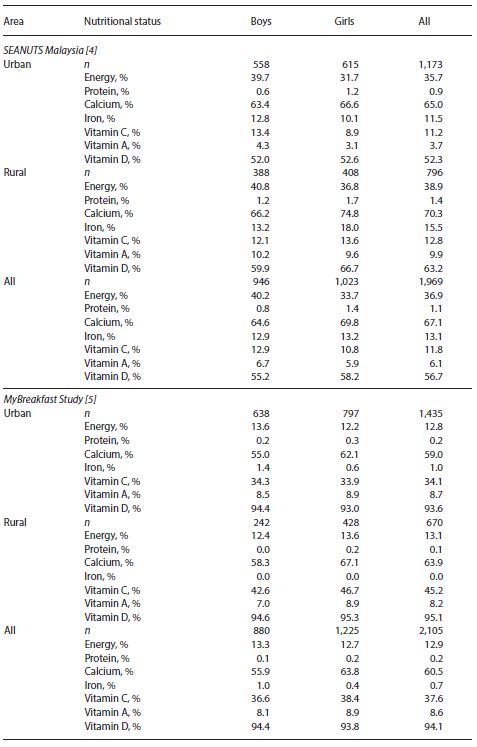
Table 2. Breakfast consumption among primary school children in Malaysia: the SEANUTS Malaysia [10] and MyBreakfast Study [9]
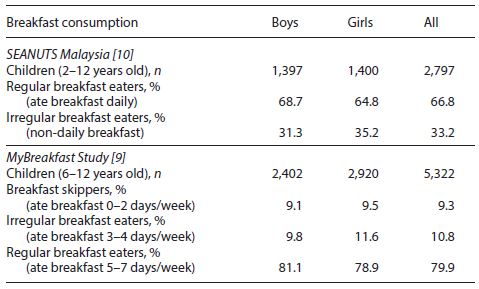
A total of 65.2% of children in the SEANUTS Malaysia consumed breakfast daily. Regular breakfast eaters were found to have higher intake of calcium and vitamins A, C, and D than irregular breakfast eaters [3]. Analysis of 2-day dietary recalls from the MyBreakfast study showed that 17.7% of the children consumed ready-to-eat cereal (RTEC) at breakfast, while among non-RTEC consumers, bread (44.2%), eggs (31.8%) and nasi lemak (23.9%) were the most common foods consumed at breakfast [4]. RTEC was found to be the major contributor of whole grain (68.6%), followed by hot cereal (18.6%), biscuits (8.7%), and bread (1.8%) [5]. It was also shown that only 1.0% of Malaysian children achieved the 43 g/day of whole grain intake recommendation in the Malaysian Dietary Guideline (MDG) for children and adolescents.
In the SEANUTS Malaysia, among children aged 7–9 years (n=890), only 13.4 and 9.5% met the MDG for fruits and vegetables per day, respectively. The pattern was similar among the older children aged 10–12 years (n=883), although slightly higher, whereby only 19.6 and 16.1%, respectively, met the MDG for fruits and vegetables. For the milk group, only very low percentages (5.5%) of children aged 7–9 years and among those aged 10–12 years (3.7%) met the MDG for milk/dairy products [4]. Despite the low milk drinking habits, the MyBreakfast study showed that UHT (ultraheat-treated) milk was commonly consumed at breakfast among RTEC consumers [5]. Thus, the consumption of RTEC at breakfast can promote milk consumption among the children and, subsequently, may increase the prevalence of children meeting the MDG for milk/dairy products.
References
- Poh BK, Ng BK, Siti Haslinda MD, et al: Nutritional status and dietary intakes of children aged 6 months to 12 years: findings of the Nutrition Survey of Malaysian Children (SEANUTS Malaysia). Br J Nutr 2013;110:S21–S35.
- Tee ES, Nurliyana AR, Norimah AK, et al: Breakfast consumption among Malaysian primary and secondary school children and relationship with body weight status – findings from the MyBreakfast Study. Asia Pac J Clin Nutr 2018;27:421–432.
- Chong KH, Wu SK, Hafizah YN, et al: Eating habits of Malaysian children: findings of the South East Asian Nutrition Surveys (SEANUTS). Asia Pac J Public Health 2016;28:59S–73S.
- Koo HC, Poh BK, Lee ST, et al: Are Malaysian children achieving dietary guideline recommendations? Asia Pac J Public Health 2016;28:8S–20S.
- Mohd Nasir MT, Nurliyana AR, Norimah AK, et al: Consumption of ready-to-eat cereals (RTEC) among Malaysian children and association with socio-demographics and nutrient intakes – findings from the MyBreakfast study. Food Nutr Res 2017;61:1304692.
Breakfast: Shaping Guidelines from Food and Nutrient Patterns
Michael Gibney and Irina UzhovaThe value of regular breakfast intake for nutrition, health, and wellbeing is widely recognized. Data exist, with varying degrees of confirmation, that a regular breakfast intake may help in body weight management, in cognitive function, and in cardiometabolic health. Regular breakfast consumers also enjoy a more optimal total daily intake of nutrients compared to breakfast skippers. A critically important question that must be addressed by policy makers is the approach to defining an optimal breakfast. Such a definition would involve the enumeration of quantitative nutrient guidelines which should transcend geographic patterns and ensuing food-based dietary guidelines that would reflect local foods and gastronomic customs.
Most governments that have issued standards for optimal breakfasts have done so in the context of food groups such as cereals, breads, fruits, and fruit juices, dairy produce, and pulses. None have based their recommendations on any underlying objective evidence derived from any analysis of existing breakfast patterns. Two countries, the USA and Mexico, have issued statutory guidelines on nutrient and food choices for optimal breakfasts in schools. In both cases, the nutrient recommendations are simply energy-adjusted targets based on prevailing dietary guidelines for adults. Moreover, neither enumerates specific targets for micronutrients and neither do they elaborate on the evidence base for the targets set for food intakes to achieve these nutritional guidelines. In the UK, a voluntary nutrient standard for school meals recommends a universal figure of 20% of daily intake based on the frequently observed finding that breakfast supplies about 20% of daily energy intake. The reality is that the intakes of many desirable nutrients, the minerals and vitamins in particular, contribute far more than 20% to total daily intake.
Cluster and principal component analyses have been used to identify patterns of breakfast food intake. These studies have frequently allowed the intakes of nutrients of different breakfast food clusters to be described in terms of their contribution to both breakfast nutrients and to overall daily nutrients. What is clear from an analysis of some of these data is that intake of nutrients across clusters of breakfast foods is very large compared to the variation that exists for the same clusters as regards total daily intake. In simple terms, good breakfast patterns do not automatically lead to optimal daily nutritional patterns. Equally, poor quality of breakfast nutrients does not determine a poor overall daily nutritional pattern.
One approach which is currently being examined by the International Breakfast Research Initiative is to assign each individual in a national survey with a value for their nutrient-rich food (NRF) index. The NRF index measures dietary quality for both macro- and micronutrients and has been extensively used across the globe to provide a quantitative score of overall dietary quality. For each of 6 national surveys (Canada, Denmark, France, Spain, UK, and USA), tertiles of NRF scores are created, indicating increasing overall energy-adjusted dietary quality. The intake of foods and nutrients for each individual at breakfast is computed for each of the 3 NRF tertiles. This approach is to be explored to establish if optimal breakfast nutrient targets can be defined. As regards food-based dietary guidelines, these will alter across different gastronomic traditions, but some critically important points need to be noted before food advice for breakfasts is issued. The average population intake of a food is a function of 2 elements: the percentage of the population consuming the food and the mean intake of the food among consumers of that food. The average intake of yogurt across NRF tertiles is constant for yogurt consumers. However, as NRF scores improve, more people eat yogurt. This approach is essential for public health nutrition in improving breakfast food choice toward achieving an optimal nutrient intake.
The Importance of Dietary Protein at Breakfast in Childhood
Leonidas KaragounisProteins (derived from the Greek word πρώτειος [proteios] meaning “first one” or “most important one”) are the major functional and structural components of all the cells of the body and participate in virtually all biological processes occurring in the body. Protein provides amino acids to the body that are used to build and maintain bones, muscles, and skin, and to produce molecules with important physiological roles, such as enzymes, hormones, neurotransmitters, and antibodies. To this end, dietary protein intake is imperative in child nutrition because, unlike adults, children are in a state of ongoing growth with nutrition and exercise being the most potent stimulators of physical growth and development [1–3]. To support normal growth and this activity-induced augmentation of lean mass, adequate dietary protein ingestion is important for providing the requisite substrates to support the remodeling and growth of these lean tissues, including muscles [1]. Skeletal muscle is the most abundant tissue in the body comprising 40–50% of body mass in humans and making up a large component of the overall lean tissue component. Beyond locomotion, skeletal muscle plays a key role in central metabolism and is responsible for about 60–70% of total glucose uptake and, therefore, directly impacting metabolic health [4]. Skeletal muscle as well as the whole body protein pool is highly metabolic and undergoes rapid diurnal turnover, a process that is intricately regulated by the balance between the rates of protein synthesis and degradation. The increase in whole body protein balance is an important adaptive response to both contractile activity (i.e., exercise) and nutrient availability (i.e., protein ingestion) [4].
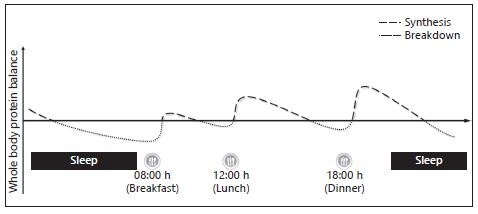
In terms of nutrient availability, current research supports the concept of nutrient timing intake. For example, the diurnal turnover of whole body protein which in turn impacts whole body protein balance (Fig. 1) may to some extent be dictated by specific need states where macronutrient intake such as protein and carbohydrates may be imperative to support healthy physical growth and development. Specifically, similar to
References
- Rodriguez NR: Optimal quantity and composition of protein for growing children. J Am Coll Nutr 2005;24:150S–154S.
- Tobias JH, Steer CD, Mattocks CG, et al: Habitual levels of physical activity influence bone mass in 11-year-old children from the United Kingdom: findings from a large population-based cohort. J Bone Miner Res 2007;22:101–109.
- Baxter-Jones AD, Eisenmann JC, Mirwald RL, et al: The influence of physical activity on lean mass accrual during adolescence: a longitudinal analysis. J Appl Physiol 2008;105:734–741.
- Karagounis LG, Hawley JA: Skeletal muscle: increasing the size of the locomotor cell. Int J Biochem Cell Biol 2010;42:1376–1379.
Breakfast Consumption versus Breakfast Skipping: The Effect on Nutrient Intake, Weight, and Cognition
Carol E. O’Neil and Theresa A. NicklasFoods consumed at the breakfast meal are culturally different, but to most individuals, when they hear the local word for “breakfast,” it is understood what is meant. However, for researchers, nutrition educators, and nutrition policy makers there is no standard definition of breakfast, breakfast consumers, or breakfast skippers. This hinders interpretation of individual articles and makes it difficult to compare the literature. It has also led to conflicting results, compounding the difficulty for educators and policy makers to make recommendations for what to consume at breakfast.
Breakfast has also been heralded as the “most important meal of the day,” not only because it is for most people the first major eating episode after the longest period without eating, but because it has been championed as a meal that contributes significantly to nutrient intake, can be used to lose weight or maintain a weight loss, and improve cognition and school performance in children. But is it the most important meal? There are two considerations here – what does “important” mean? Again, there is no definition. Further, how does the contribution of the breakfast meal to nutrient intake, weight management, or cognition compare with other meals and snacks? Breakfast has been intensively studied – lunch, dinner, and snacks, less so.
How breakfast consumption or breakfast skipping is defined influences the results of studies. In general, nutrient intake and diet quality is better if breakfast is consumed. Weight and weight management also depends on the type of breakfast consumed. It has been demonstrated clearly that the type of breakfast consumed affects nutrient intake, diet quality, and weight; therefore, a simple definition of “breakfast” does not significantly add to the literature. Less well defined is the role breakfast plays in the cognition of students. Although accepted as fact, results evaluating acute and chronic consumption of breakfast and cognition are equivocal. Systematic reviews and one carefully conducted clinical trial have suggested that there is no association between consumption of breakfast and cognition in school-age children.
More carefully controlled studies that use a standardized definition of breakfast consumption and breakfast skipping are needed to determine the effects of nutrient intake, health parameters, and academic performance. In addition, equivalent studies of the lunch and dinner meals are also needed, before it can be determined if “breakfast is the most important meal of the day.”
Suggested Reading
- Adolphus K, Bellissimo N, Lawton CL, et al: Methodological challenges in studies examining the effects of breakfast on cognitive performance and appetite in children and adolescents. Adv Nutr 2017;8:184S–196S.
- Adolphus K, Lawton CL, Champ CL, et al: The effects of breakfast and breakfast composition on cognition in children and adolescents: a systematic review. Adv Nutr 2016;7:590S–612S.
- Adolphus K, Lawton CL, Dye L: The effects of breakfast on behavior and academic performance in children and adolescents. Front Hum Neurosci 2013;7:425.
- Betts JA, Chowdhury EA, Gonzalez JT, et al: Is breakfast the most important meal of the day? Proc Nutr Soc 2016;75:464–474.
- Brown AW, Bohan Brown MM, Allison DB: Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am J Clin Nutr 2013;98:1298–1308.
- Cho S, Dietrich M, Brown CJ, et al: The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr 2003;22:296–302.
- Crossman A, Anne Sullivan D, Benin M: The family environment and American adolescents’ risk of obesity as young adults. Soc Sci Med 2006;63:2255–2267.
- Deshmukh-Taskar PR, Nicklas TA, O’Neil CE, et al: The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999–2006. J Am Diet Assoc 2010;110:869–878.
- Dhurandhar EJ, Dawson J, Alcorn A, et al: The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014;100:507–513.
- Dietary Guidelines for Americans 2010. https://health.gov/dietaryguidelines/dga2010/ dietaryguidelines2010.pdf (accessed February 10, 2018).
- Dietary Guidelines Advisory Committee Report 2015–2020. https://health.gov/ dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015Dietary-Guidelines-Advisory-Committee.pdf (accessed February 10, 2018).
- Dietary Guidelines for Americans 2015–2020. https://health.gov/dietaryguidelines/2015/ guidelines (accessed February 10, 2018).
- Edefonti V, Rosato V, Parpinel M, et al: The effect of breakfast composition and energy contribution on cognitive and academic performance: a systematic review. Am J Clin Nutr 2014;100:626–656.
- Frank GC: Breakfast: what does it mean? Am J Lifestyle Med 2009;3:160–163.
- Giovannini M, Verduci E, Scaglioni S, et al: Breakfast: a good habit, not a repetitive custom. J Int Med Res 2008;36:613–624.
- Hoyland A, Dye L, Lawton CL: A systematic review of the effect of breakfast on the cognitive performance of children and adolescents. Nutr Res Rev 2009;22:220–243.
- Iovino I, Stuff J, Liu Y, et al: Breakfast consumption has no effect on neuropsychological functioning in children: a repeated-measures clinical trial. Am J Clin Nutr 2016;104:715–721.
- Kerver JM, Yang EJ, Obayashi S, et al: Meal and snack patterns are associated with dietary intake of energy and nutrients in US adults. J Am Diet Assoc 2006;106:46–53.
- Nicklas TA, Reger C, Myers L, et al: Breakfast consumption with and without vitamin-mineral supplement use favorably impacts daily nutrient intake of ninth-grade students. J Adolesc Health 2000;27:314–321.
- Nooyens AC, Visscher TL, Schuit AJ, et al: Effects of retirement on lifestyle in relation to changes in weight and waist circumference in Dutch men: a prospective study. Public Health Nutr 2005;8:1266–1274.
- O’Neil CE, Byrd-Bredbenner C, Hayes D, et al: The role of breakfast in health: definition and criteria for a quality breakfast. J Acad Nutr Diet 2014;114(12 suppl):S8–S26.
- O’Neil CE, Nicklas TA, Fulgoni VL 3rd: Nutrient intake, diet quality, and weight/adiposity parameters in breakfast patterns compared with no breakfast in adults: National Health and Nutrition Examination Survey 2001–2008. J Acad Nutr Diet 2014;114(12 suppl):S27–S43.
- O’Neil CE, Nicklas TA, Fulgoni VL 3rd: Nutrient intake, diet quality, and weight measures in breakfast patterns consumed by children compared with breakfast skippers (NHANES) 2001–2008. AIMS Public Health 2015;2:441–468.
- O’Neil CE, Zanovec M, Nicklas TA, et al: Pre-sweetened and non-pre-sweetened readyto-eat cereals at breakfast are associated with improved nutrient intake but not with increased body weight of children and adolescents: NHANES 1999–2002. Am J Life Med 2012;6:63–74.
- Priebe MG, McMonagle JR: Effects of ready-to-eat-cereals on key nutritional and health outcomes: a systematic review. PLoS One 2016;11:e0164931.
- Rampersaud GC, Pereira MA, Girard BL, et al: Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005;105:743–760.
- School Breakfast Program. https://www.ers.usda.gov/topics/food-nutrition-assistance/ child-nutrition-programs/school-breakfast-program (accessed February 10, 2018).
- United States Department of Agriculture/Agricultural Research Service: What We Eat in America. https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-humannutrition-research-center/food-surveys-research-group/docs/wweia-data-tables (accessed February 10, 2018).
- Wyatt HR, Grunwald GK, Mosca CL, et al: Long-term weight loss and breakfast in subjects in the National Weight Control Registry. Obes Res 2002;10:78–82.
Breakfast, Glycemic Index, and Cognitive Function in School Children: Evidence, Methods, and Mechanisms
Sandra I. Sünram-LeaBreakfast has been claimed to improve cognitive function and academic performance, leading to the provision of breakfast initiatives by public health bodies. Children may be particularly sensitive to the nutritional effects of breakfast due to greater energetic needs compared to adults. However, there is a lack of acute intervention studies assessing what type of breakfast is optimal for cognitive performance. Dietary carbohydrates are of interest as they provide the main source of energy for the brain’s metabolic functioning, and there is mechanistic evidence linking postprandial glycemia to cognitive performance in both children and adult populations [1]. Therefore, when considering what type of breakfast may be beneficial, the rate at which breakfast increases and maintains blood glucose, i.e., “the glycemic index” (GI) might be an important factor. Related to this is the concept of glycemic load (GL), which takes the amount of carbohydrates consumed into account. A review of studies investigating the optimal rate of glucose supply following breakfast consumption suggests that a lower postprandial glycemic response may be protective against a decline in cognitive performance over the morning. More specifically, findings to date suggest that beneficial effects of a low-GI or -GL breakfast are usually observed later in the morning. In terms of aspects of cognition, a low-GI or -GL breakfast was most consistently associated with beneficial effects on attention, but beneficial effects in memory and executive function have been observed [2]. Although the evidence to date is promising, it is currently insufficient to allow firm and evidence-based recommendations. What limits our ability to draw conclusions from previous findings is that the studies have differed widely with respect to subject characteristics (age, sex, and habitual breakfast consumption), cognitive tests used, and timing of cognitive assessment. In addition, few studies have profiled glycemic response in children [3, 4]. There is, therefore, an urgent need for
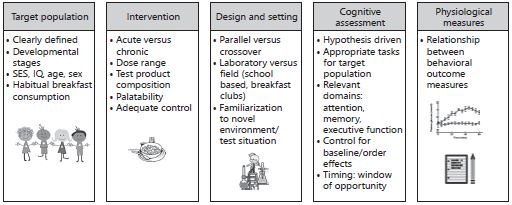
hypothesis-driven, randomized, controlled trials that evaluate the role of different glycemic manipulations on cognition. These should incorporate cognitive tasks that are sensitive to nutritional manipulations but also relevant to the specific learning situation encountered. Moreover, for future studies, multiple assessments at various time points, including baseline assessment and testing in the later period of the morning, are necessary to reveal the effects and time course of glycemic effects on cognition. Furthermore, there is a clear lack of intervention studies that employ ecologically valid research conditions, such as school-based testing. In addition, more data are needed in terms of the glycemic response to breakfast manipulation in children. These will also help to clarify the nature of the relationship between postprandial blood glucose concentrations and cognition (see Fig. 1 for important conceptual and methodological considerations when carrying out research into the effects of breakfast on cognition). Understanding the potential influence of breakfast interventions on children’s cognitive function remains a high priority given its application to learning and achievement at school. To date, the evidence is insufficient to allow firm conclusions as to what type of breakfast is most beneficial, but low-GI or -GL breakfasts which result in a lower postprandial glycemic response might be a promising strategy to optimize performance across the morning. However, further work is needed to substantiate this notion.
References
- Sünram-Lea SI, Owen L: The impact of diet-based glycaemic response and glucose regulation on cognition: evidence across the lifespan. Proc Nutr Soc 2017;76: 466–477.
- Adolphus K, Lawton CL, Champ CL, Dye L: The effects of breakfast and breakfast composition on cognition in children and adolescents: a systematic review. Adv Nutr 2016;7:590S–612S.
- Brindal E, Baird D, Danthiir V, et al: Ingesting breakfast meals of different glycaemic load does not alter cognition and satiety in children. Eur J Clin Nutr 2012;66:1166–1171.
- Brindal E, Baird D, Slater A, et al: The effect of beverages varying in glycaemic load on postprandial glucose responses, appetite and cognition in 10–12-year-old school children. Br J Nutr 2013;110:529–537.
List of Speakers
Dr. Imelda Angeles-Agdeppa
Nutrition Assessment and
Monitoring Division
Food and Nutrition Research
Institute (FNRI)
Department of Science and
Technology (DOST)
General Santos Avenue
Taguig, 1630 Metro Manila
Philippines
E-Mail iangelesagdeppa@yahoo.com.ph
Prof. Regan Bailey
Department of Nutrition Science
Purdue University
700 W State Street
West Lafayette, IN 47 907
USA
E-Mail reganbailey@purdue.edu
Dr. Alison L. Eldridge
Nestlé Research
Vers-Chez-les-Blanc
CH–1000 Lausanne 26
Switzerland
E-Mail Alison.Eldridge@rdls.nestle.com
Dr. Ciarán G. Forde
Clinical Nutrition Research Centre
(CNRC)
A*STAR
Singapore Institute for Clinical
Sciences (SICS)
Yong Loo Lin School of Medicine
National University of Singapore
14 Medical Drive 07-02, MD 6
Building
Singapore 117599
Singapore
E-Mail ciaran_forde@sics.a-star.edu.sg
Dr. Lisa Fries
Nestlé Research
Vers-Chez-les-Blanc
CH–1000 Lausanne 26
Switzerland
E-Mail Lisa.Fries@rdls.nestle.com
Prof. em. Mike Gibney
Institute of Food and Health
University College Dublin
Belfield, Dublin 4
Ireland
E-Mail mike.gibney@ucd.ie
Prof. Christiani Jeyakumar Henry
Clinical Nutrition Research Centre
(CNRC)
A*STAR
Singapore Institute for Clinical
Sciences (SICS)
Yong Loo Lin School of Medicine
National University of Singapore
14 Medical Drive 07-02, MD 6
Building
Singapore 117599
Singapore
E-Mail jeya_henry@sics.a-star.edu.sg
Dr. Leonidas G. Karagounis
Musculoskeletal Physiology Group
Nestlé Research
Vers-Chez-les-Blanc
CH–1000 Lausanne 26
Switzerland
E-Mail Leonidas.Karagounis@rdls.nestle.com
Prof. Dr. Norimah A. Karim
Nutrition Science Programme
School of Health Sciences
Faculty of Health Sciences
Universiti Kebangsaan Malaysia
Jalan Raja Muda Abd Aziz
50300 Kuala Lumpur
Malaysia
E-Mail norimahkarim@ukm.edu.my
Prof. Dr. Andrea Maier-Nöth
Eat-Health-Pleasure GmbH
Psychology of Eating, Health and
Nutrition
Hauptstrasse 14a
CH–8280 Kreuzlingen
Switzerland
E-Mail andrea.maier@eat-health-pleasure.com
Dr. Kimberley Mallan
School of Psychology
Australian Catholic University
1100 Nudgee Road
Banyo, QLD 4014
Australia
E-Mail Kimberley.Mallan@acu.edu.au
Prof. Theresa A. Nicklas
USDA Agriculture Research Services
Children's Nutrition Research
Center
Baylor College of Medicine
1100 Bates Avenue
Houston, TX 77030
USA
E-Mail tnicklas@bcm.edu
Dr. Sophie Nicklaus
Institut National de la Recherche
Agronomique (INRA)
UMR1324 Centre des Sciences du
Goût et de l'Alimentation
17 rue Sully
FR–21000 Dijon
France
E-Mail Sophie.nicklaus@inra.fr
Dr. Sandra I. Sünram-Lea
Metabolic Regulation and Cognition
Laboratory
Department of Psychology
Lancaster University
Lancaster, LA1 4YF
UK
E-Mail s.sunram-lea@lancaster.ac.uk
Prof. Salvador Villalpando-Carrión
Pediatric Gastroenterology and
Nutrition
Hospital Infantil de México
Frederico Gómez
Universidad Nacional Autonoma de
Mexico
Calle Dr. Marquez No. 162.
Cuauhtemoc 06720, Ciudad de
México
Mexico
E-Mail Salvador.Villalpando@mx.nestle.com
Dr. Dantong Wang
Nestlé Research
Vers-Chez-les-Blanc
CH–1000 Lausanne 26
Switzerland
E-Mail Dantong.Wang@
rdls.nestle.com
© 2019 Nestlé Nutrition Institute, Switzerland
CH 1814 La Tour-de-Peilz.
All rights reserved. Unless special permission in writing is obtained, no part of this publication may be reproduced, stored in a retrieval system, or be transmitted in any form or by any means, electronic, mechanical, photo copying or otherwise.
The material contained in this issue was submitted as previously unpublished material, except in the instances in which credit has been given to the source from which some of the illustrative material was derived. Nestlé Nutrition Institute cannot be held responsible for errors or omissions, or for any consequences arising from the use of the information contained herein.
If you liked this post you may also like