Plant based drinks in the diets of infants and young children
Cow’s milk (CM) is traditionally a part of the western diet for toddlers and young children as a source of protein, calcium and other nutrients. While it is not a requirement in a child’s diet, it was seen in recent studies that it has an impact on a child’s growth, where those who do not drink CM grow at a slower rate than those who do. With the emergence of plant-based diets, plant-based drinks (PBD) have also been consumed more. For infants, plant-based infant formula such as soy and rice hydrolysate-based formulas are used for medical and ethical reasons. While the role of specific PBD in children’s diets have yet to be determined, their impact needs to be assessed in the context of their percent of the diet, child age, health status, nutritional requirements and the composition of the rest of the diet, especially as plant-based diets continue to gain traction. Other recommendations also include improvements in available alternative drinks and more informative labelling of such products.
ABSTRACT
Plant based drinks (PBD) do not have a role in providing nutrition to infants, other than the feeding of commercial soy and rice hydrolysate based infant formulas for medical, religious or ethical reasons. For toddlers and young children, cow’s milk (CM) has a traditional place in their modern Western diet as an important source of protein, calcium and other nutrients. While milk is not essential to provide a healthy diet for young children, considerable dietary adjustments need to be made to compensate for its absence. Most PBD are not equivalent to CM in terms of inherent nutrient content and bioavailability and are more expensive. There is notable heterogeneity in their nutritional composition. According to recent studies, children who do not drink CM grow slower than those who do. There is relatively little information about the role of specific PBD in children’s diets. Their impact needs to be assessed in the context of their percent of the diet, child age, health status, nutritional requirements and the composition of the rest of the diet. There are both questionable and valid reasons consumers and parents drink and provide PBD to young children, including misinformation, medical conditions, worries about toxins in CM and ethical/religious beliefs. Parents, and consumers in general, are increasingly acting on concerns about animal welfare related to modern farming practices and the adverse environmental impact of meat and dairy farming. Improvements in available alternative drinks and more informative labelling of such products are likely to be welcomed by the marketplace. The new technology of precision fermentation has the potential to lead to milk alternatives that address many of the concerns about both CM and PBD.
INTRODUCTION
There are important nutritional differences among plant based drinks (PBD) and between them and the cow’s milk (CM) they may replace in the diets of children. These differences have been competently documented by a number of authors, on whose work this manuscript relies.1–5 The North American Society for Pediatric Gastroenterology, Hepatology and Nutrition has identified nutritional concerns about the inappropriate use of PBD for children.6 Workers in other fields have examined the environmental impact of growing plants versus dairy and meat farming and ethical frameworks that exclude animal products from human diets. This review article seeks to place what we know about the nutrition of CM and alternative PBD in the context of the reasons parents give for choosing PBD for their children.
Role of CM in the diets of children
In societies that farm milk-producing animals, animal milk has long been part of the diet, including the diet of children. Global milk availability has increased since advances in milk processing in the 19th century led to shelf-stable packaged milk products. The expansion of refrigeration in the early 20th century made safe fresh liquid milk more generally available in higher income countries. While thoughtful parents can provide children with a complete and healthy diet in the absence of CM or other animal milk,7 it can be difficult to meet all of children’s needs with a vegan diet.8 This may be especially true when other foods in the diet come from a narrow range of foods due to availability, selective food purchasing or selective eating behaviour.
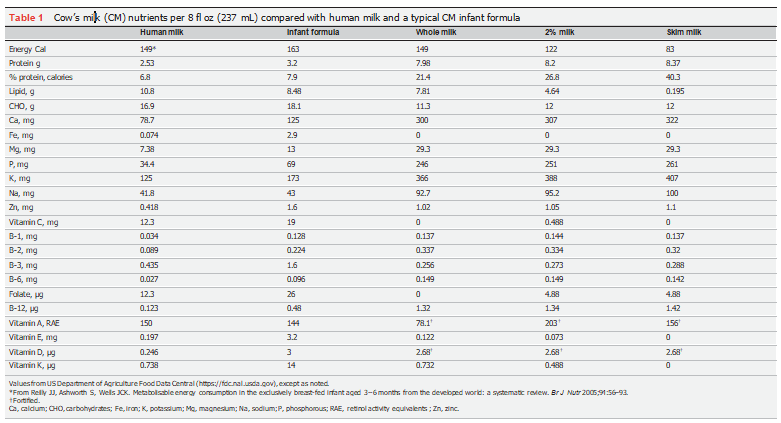
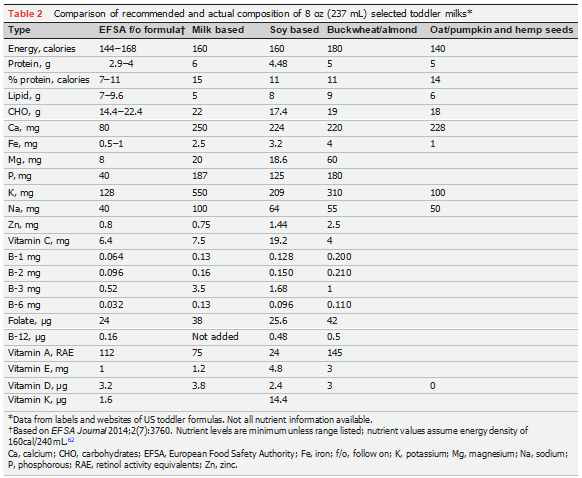
CM is commonly added to the toddler diet after the first birthday. It can replace breast milk or formula as the liquid source of nutrition in the diet. By 1 year of age,other foods generally provide about a third of the diet. At this point, kidney function has developed such that the high protein and mineral content of CM is no longer metabolically stressful. The caloric density of CM approximates that of human milk and infant formula, but protein makes up a higher percent of the calories (table 1). Over the course of the second year of life, the United States Department of Agriculture (USDA) recommends intake of 1-2/3-2 cups of CM per day (https://ask.usda.gov/s/article/ How-much-dairy-should-I-provide-for-my- child-under-the-age-of-two-How-much-milk- should-my-child-drin). For 1-to 3-year-olds, milk is expected to contribute about 25–35% of calories (based on recommendations in https://www.myplate.gov/myplate-plan). Between ages 2 and 8 the recommendation is for 2 to 2-1/2 cups per day (https://www.cdc.gov/nutrition/InfantandToddlerNutrition/foods-and-drinks/cows-milk-and-milk-alternatives.html; Table 3-1 from https://www.dietaryguidelines.gov/sites/default/files/2021–03/Dietary_Guidelines_for_Americans-2020– 2025.pdf). The American Academy of Pediatrics recommends that toddlers should receive whole milk, and young children skim or 1% milk, although the rationale for the recommendations for skim milk has been seriously challenged.9 10 Infants in the second year of life are at risk of poor intakes of iron, zinc, vitamin D and essential fatty acids. Nutritionally, milk complements other foods in the diet at this age.6 The match is imperfect.11 Given the high density of many nutrients in CM, it remains an important part of most Northern Hemisphere early childhood diets, particularly for providing protein, minerals and selected vitamins, including vitamins A and D, when the milk is fortified.12 In Europe, young child milks are used in some countries as an alternative to CM, with their nutritional composition thought better to complement the diet of toddlers and young children.11 The European Society for Paediatric Gastroenterology Hepatology and Nutrition has not recommended a formulation any different from follow-on formulas. However, toddler milks are not regulated like infant formulas13 and may not always provide the nutrient levels recommended for this age group, and often contain added sugars.14 A few of these are plant based (table 2).
Studies have shown that linear growth tends to be faster in children who receive CM as part of their diet, as frequently documented in children with CM allergy.15–19 Some of this effect may be related to specific nutrients rich in CM including calcium, vitamin D and riboflavin.20 Faster growth is perceived as broadly beneficial.21 However, there are concerns about potential deleterious effects of accelerated growth in certain circumstances, as it may be associated with obesity and metabolic syndrome.22
Health concerns associated with feeding CM to children
There are health reasons for not feeding CM to some children, including CM allergy, in its variety of manifestations. It is recognised in 0.5–3% of infants by 1 year of age.23 This condition tends to resolve during childhood, including early childhood, and by 6 years, 90% have achieved milk tolerance.24
There are other health concerns with feeding milk to infants and children. These include iron deficiency related to the low iron content of milk and adverse gastro-intestinal effects of milk, including blood loss in infants and anaemia with protein losing enteropathy in children given large volumes. Much of the world outside of populations native to western, southern and northern Europe becomes lactose intolerant in childhood.25 This leads to symptoms in some with milk ingestion. There are rare inborn errors of metabolism for amino acids and sugars for which CM intake is contraindicated. Infants with William’s syndrome should not receive vitamin D fortified milk.
Many chronic health conditions have not been shown to be associated with CM intake. Whole milk has not been associated with obesity or consistently with diabetes. Blood low density lipoprotein cholesterol is not more likely to be abnormal in children consuming milk. The adult disease most strongly associated with milk intake is prostate cancer, and this association includes milk intake during childhood. Others have recently described and summarised the relationship of these conditions to milk intake.9,10,26,28 It is not the purpose of this article to discuss these in detail. Acne has also been linked to CM intake, but this condition usually does not manifest until later in childhood or adolescence.
Milk provides a micronutrient dense source of calories and protein. Ingestion of CM with its high levels of branched-chain amino acids, milk insulin-like growth factor-1 (IGF-1), lactose, and micro RNA stimulates insulin secretion and hepatic IGF-1 release. This activates tissue mechanistic target of rapamycin complex 1 (mTORC1) and its associated anabolic and other (potentially adverse) effects.28 mTORC1 functions as a signalling mechanism related to control of tissue growth, metabolism, inflammation and autophagy. Chronic milk ingestion may alter metabolism in the direction of insulin resistance.28 In early life, this mTORC1 stimulation is central to the growth and development process. Interestingly, these mTORC1 pathophysiologic mechanisms do not appear to be activated by dairy products subjected to fermentation, which substantially changes the nutrient characteristics of the milk.
CM can bring with it substances unrelated to its nutritional composition. These include antibiotics, hormones, pesticides and other toxins.29 Recent US data in this regard are reassuring relative to the low frequency of antibiotic detection30 (https://www.nmdrd.com/fy-21. pdf). Of note, US organic milk rarely showed any presence of antibiotics. In some other parts of the world, anti-biotic residues in CM appear to be more common and of medical and public health concern.29,31,32 Exposure to these potential contaminants can be reduced by use of organic milk.
Much of the commercial non-organic milk produced in the USA comes from cows treated with bovine somatotropin (BST). Administered BST does not transfer to milk, is digested by stomach acid (https://www.fda.gov/animal-veterinary/product-safety-information/bovine-somatotropin-bst) and is not bioactive.33 However, the milk from BST treated cows has higher levels of IGF- 1,30 which can be bioactive, at least in the gastrointestinal tract.34 Concerns specific to BST and its associated higher IGF-1 content can be addressed with the selection of milk from non-BST treated cows and organic milk.
Dairy cows are commonly pregnant while milked, and pregnancy related sex hormones transferred to milk appear to be bioactive.35 Studies have shown associations of CM intake and some later adulthood sex-hormone sensitive malignancies, possibly related to milk hormones and/or the metabolic effects of CM ingestion.9, 28
PBD
There is no regulatory standard of identity for the composition of PBD. PBD can be based on legumes (soybeans, peas), seeds (hemp, sunflower), nuts (almond, pecan, macadamia), grains (rice, oats) and pseudo-grains (quinoa, buckwheat). The beverage protein is provided by one or more of these plant sources, and they contribute other nutrients and properties to the milk. The extensive processing necessary to convert these foods to milks includes soaking, grinding, blanching, separation procedures, homogenisation, thermal processing and formulation during which nutrients and other ingredients—usually including sugar and salt2—are added to achieve appearance, taste and mouth feel more closely resembling CM.2, 36 The process varies with the starting plant source or plant protein source and the desired final product attributes. The bioavailability of nutrients in PBD is usually less than that for CM due to lower digestibility and factors such as phytates that interfere with nutrient absorption.37 These anti-nutritional factors are variably affected by food processing. Food manufacturers may make more than a single milk product from a plant source, for example, almond milk with or without added sugar. Some PBD are formulated to come close to the composition and properties of CM, and others are made without additives or fortification. PBD may be available in shelf stable, refrigerated and powder formats and in bulk or single serve packaging. Some are certified organic or use organic ingredients.
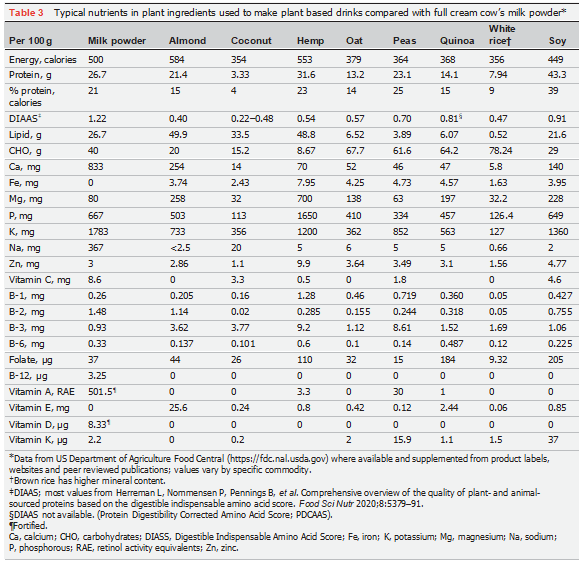
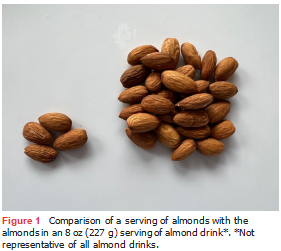
The plant sources used for PBD are lower in multiple— and variable—essential amino acids, compared with animal protein sources, reflected in part by the lower Digestible Indispensable Amino Acid Score (DIAAS), and may contain anti-nutritional factors that can interfere with nutrient absorption. However, the foods from which PBD are derived play a nutritious and healthy role in the diet (table 3). The same is less often true for the derived PBDs. As an example, almonds are rich in protein, mono- and polyunsaturated fatty acids, minerals and some B vitamins and can be part of a healthy diet. A 1 oz (28 g) serving of almonds is about 28 almonds. In contrast, a cup of many of the commercial almond milks provides the protein equivalent of four almonds (figure 1). Sugar may be added for flavour and vegetable oils for energy and essential fatty acids. Fortification is often the source of many of the nutrients claimed on the nutrition label. Fortified nutrients, notably calcium, have uncertain physical stability and bioavailability in the final matrix. Fermentation of plant ingredients, and including more than one plant source, may improve taste and nutrient content and availability.
The production of PBD generally requires sophisticated food processing machinery and know-how, making plant milks more expensive than CM.38 PBD may be categorised as ultra-processed drink products using the NOVA system of food classification.39 NOVA was developed in support of the United Nations Sustainable Development Goals and provides one means for categorising foods relative to their contribution to diet quality, impact on malnutrition and the sustainability of food systems.40 Ultra-processed foods are manufactured from substances derived from foods and other organic sources and are ready-to-consume. They often contain flavouring agents, stabilisers, colouring agents and food processing aids such as emulsifiers. Ultra-processed foods now make up a high percentage of the diet of high-income (developed) countries (estimated at 67% for US youth)41 and an increasing percentage of the diet of low- and middle-income (developing) countries.42 Epidemiologic studies link ultra-processed foods to poorer diet quality and the rising level of chronic non-communicable diseases including obesity, dyslipidaemia and metabolic syndrome.42 Avoidance of minimally processed CM in favour of PBD, that may be classified as ultraprocessed, may entail its own potential diet-related morbidity or add to any attributable to ultra- processed foods. Some countries are now implementing efforts to suppress the incursion of ultra-processed foods into their food supply.
Plant based infant formulas and PBD for infants
For infants, the universally preferred and recommended milk is own mother’s milk. Current recommendations are for feeding human milk for at least 6 months and up to 2 years or longer.43 Adherence to these recommendations is variable from country to country and within countries related to breast milk supply, maternal preferences and socioeconomic variables, including employment outside of the home and formula marketing practices. Most US infants receive a milk other than breast milk before the end of the first year of life.44 When available, the recommended breast milk substitute for infants is an iron-fortified CM based commercial infant formula. Through the first year of life, breast milk and/or infant formula remain the dominant and preferred source of nutrition. Unmodified CM is not recommended in the first year of life due to its much higher protein and mineral content, the relatively low absorption of butter fat, the low content of essential and long chain polyunsaturated acids, its low iron and zinc content, and its association with faecal blood loss.
Few plant based protein sources have been utilised to manufacture infant formulas. Soy protein has an extended history of safe use. More recently, rice protein hydrolysate formulas have become available in a few European countries. Plant based infant formulas are not the first choice for infants with CM allergy.24 45 However, soy formula is effective for managing immunoglobulin E (IgE)-mediated CM allergy. Rice protein hydrolysate formulas can be used in all forms of CM allergy. Both are suitable alternatives when parents want a vegan formula for their infant. They can also be used in galactosaemia and alactasia, as they are lactose- and galactose-free. Some expert groups advise that soy formulas not be fed to infants less than 6 months of age.24 Low level concern persists regarding possible adverse effects of the phytoestrogens in soy formula on female reproductive development.46
Marketed soy protein based and rice hydrolysate based formulas are supplemented with their limiting amino acids to bring their protein quality closer to CM. Soy formula contains added methionine, and rice hydrolysate formula contains added lysine, threonine and tryptophan. Both support satisfactory weight and length gain when provided as the sole source of milk.47 48 Soy protein meets the protein efficiency ratio quality factor for US infant formulas under the Infant Formula Act, and soy and rice hydrolysates are approved protein sources for infant formulas under European Union (EU) regulations. Multiple adverse events have been reported, including malnutrition and micronutrient deficiencies, in infants fed other PBD not meeting nutritional standards for infant formulas.49 Other specific adverse metabolic events have been associated with specific PBD, for example, oxalate kidney stones and metabolic alkalosis with almond milk. Concern persists regarding the arsenic content of some rice milks. Given the strong global recommendations for breastfeeding in infancy, the general availability of commercial infant formulas in high- and middle-income countries, and the mismatch of infant nutritional needs with the nutritional profile of most PBD, other than commercial soy and rice hydrolysate infant formulas, PBM have no nutritional role to play in the infant diet.
PBD for toddlers and young children
PBD are not generally designed specifically for children. The few US products that are marketed for children range from nutritionally complete to lacking in multiple nutrients present in CM. PBD have to taste good or children will have to be very hungry to accept them. However, making beverages sweet or improving taste with salt are not advantageous to health. Making alternative drinks that are both healthy and attractive to children has long been a challenge in developing nutritious alternative drinks for this age group.
PBD do not generally match CM in nutrient content, quality and bioavailability, except for iron, which CM lacks. A consortium of expert groups in North America advised against the use of PBD to replace milk in the diet of toddlers and young children (https://healthyeatin gresearch.org/wp-content/uploads/2019/09/HER-Heal thyBeverageTechnicalReport.pdf). Including PBD as a snack food or occasional beverage has little impact on the total diet. With the exception of soy, and a combined plant based protein toddler drink, using them as a replacement for CM poses variable nutritional challenges relative to making up the nutrients that would have been contributed by milk. Simply increasing the intake of plant based foods, without making thoughtful compensatory dietary adjustments, has the potential to place persons at risk for low intakes of calcium, protein, vitamin A and vitamin D.50 Low iodine content is also of concern in PBD, as CM is a major dietary source, but fluoride content tends to be higher in PBD.
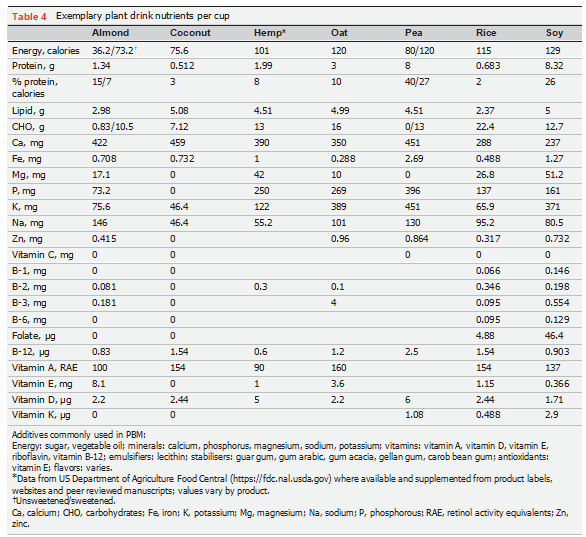
Generally, studies of vegan children find a lower prevalence of obesity, but evidence of nutrient insufficiency and slower linear growth compared with other children.8, 51 Not much has been written specifically about the nutritional impact of PBD and their contribution to nutritional status and growth of children. Given the heterogeneity of PBD, each would have to be studied in its own right to generate actionable nutritional information. In the EU and Canada, PBD are labelled as beverages rather than as milk. In the USA, it appears that manufacturers can continue to use the term ‘milk’ to describe PBD, but the label may need to clarify aspects of their nutrient content relative to CM (https://www.federalregister.gov/documents/2023/02/23/2023–03513/labeling-of-plant- based-milk-alternatives-and-voluntary-nutrient-state- ments-draft-guidance-for). Tables 1 and 4 demonstrate the mismatch in the composition of CM and PBD. There is less complete information about the micronutrient content of PBD.1,52 Energy and protein digestibility content and amino acid scores are variable and generally less than for CM.1 Soy milks generally come closest. As of 2015, there were an estimated 150 PBD available in Europe.53 Given PBD variability and the often limited nutritional information at the product-specific level, statements about the nutritional role of PBD as a group have the potential to be misleading.
Vegan consumerism and preferences for PBD
There are three common reasons for why plant based foods may be preferred over milk and other animal foods (https://www.veganfriendly.org.uk/articles/ethics- of-veganism/).54 These are (1) ethical and/or religious concerns regarding the treatment of farm animals, (2) environmental and sustainability concerns related to the local or planetary impacts of dairy (and other) animal farming with associated climate rights and intergenerational justice issues, and (3) health reasons including real or perceived illness or risk of future illness related to milk and other animal products and/or endorsement of health benefits of a plant based diet.
Animal welfare motivation
Concern over animal welfare, including dairy cows, is a strong motivator of vegan food choices. This concern is informed by increasing evidence of farm animals’ ability to experience pain, suffering and the anticipation of pain, which has led to new perspectives on animal rights.54 The degree of reduction or avoidance of eating animal products lies on a spectrum including reducetarians and flexitarians, who try to eat less animal products, ostrovegans, pescatarians, vegetarians and ultimately vegans, who seek to avoid eating all animal products54 (see vegan friendly website cited above). Veganism can be a personal practice or one involving activism for its cause, a distinction important to some ethicists who look at the efficacy of a practice as the determinant of its ethical value. Some vegans’ perspectives are nuanced by beliefs that health benefits of consuming animal products for a subset of the population (eg, CM for children at risk of impaired growth or malnutrition) outweigh otherwise cogent ethical animal welfare and/or environmental concerns.54
Environmental impact motivation
There are at least a billion cows in the world. One quarter of these are dairy cows. These have local (particularly water quality and eutrophication) and global environmental impacts. The dairy sector is estimated to be responsible for 4% of anthropometric greenhouse gases (https://www.fao.org/3/k7930e/k7930e00.pdf). Ruminants and their manure produce 6% of total global methane emissions.55 Methane is a far more potent gas for global warming than is carbon dioxide, but unlike carbon dioxide it breaks down much faster with a half- life of 8.6 years.56 Milk production also requires much more land and water than growing an equivalent amount of protein in plants, and thus decreases land and water availability for other purposes and is less sustainable.57 The few studies of the environmental impact specific to PBD confirm their environmental impact advantages. Reducing milk—and meat—production and their environmental impact is an important consideration for reducing global warming and a motivator for some who adopt a vegan diet56 (see vegan friendly website cited above). However, in the production of all types of foods, even within categories, there is a large range of environmental impacts, highlighting substantial gains to be made by achieving best agricultural practices.57
Consumer preferences
In a US national sample of parents, most parents favoured CM over PBD58; 22–41% of North American households buy PBD, often not exclusive of dairy products (https:// plantbasednews.org/news/41-us-households-buy-vegan- milk/).59 60 The most popular PBD are almond, oat and soy milks. Since available evidence indicates <3% of the population adheres to a vegan diet, these beverages have a far broader consumer appeal than just the vegan popu- lation. In a marketing study of adults, reasons for selecting PBD included taste, health benefits, value, source of nutrients and being all natural (https://www.fooddive. com/news/consumers-reveal-why-they-buy-plant-based- dairy-alternatives/516702/). In the US national sample study, concerns expressed about CM included the pres- ence of hormones and antibiotics and the environmental impact of dairy farming. A focus group study of Canadian parents identified concerns regarding toxins in CM and the environmental effects of dairy farming.60 A study of parents of young children in Miami, Florida found 88% of the parents surveyed believed PBD are nutritionally equivalent or superior to CM. Most were unaware of their energy and protein content. The Canadian study also found parental knowledge deficits regarding PBD.
Beyond PBD
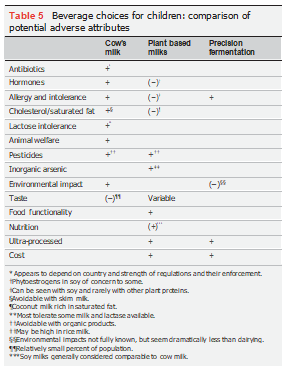
The attraction for alternatives to CM largely relate to unwanted components of CM and concerns about animal welfare and the environmental impact of dairying, as opposed to any inherent value of turning plants into a beverage resembling milk. The emerging business of precision fermentation offers a novel source of milk proteins with potential to address these concerns. In this technology, genes controlling the synthesis of a CM protein are transferred to yeast. By way of example, b-lactoglobulin can be produced by cultures of the yeast, Tricoderma reesei.61 Yeast with transferred bovine b-lacto- globulin genes are grown in large fermentation vats. The yeast-synthesized milk proteins are centrifuged, separated, cleaned and dried into a protein powder for use in alternative dairy products. While these proteins remain allergenic, they are free of lactose, cholesterol, hormones, pesticides and antibiotics. Dairy farming is not required for their production. The fermented proteins have the nutritional quality and the functionality of the corresponding CM protein.61 To date, fermented milk proteins have been used in dairy products such as cream cheese and ice cream, but not in alternative milks (https://www. msn.com/en-us/news/us/moooove-over-how-single- celled-yeasts-are-doing-the-work-of-1500-pound-cows/ar- AA18vZBH). This technology provides protein, but other ingredients are needed to make a beverage. As a result, milk beverages made from these proteins may turn out to be in the NOVA ultra-processed category. The cost of proteins made by precision fermentation will need to become more competitive with current commodities, unless subsidised to achieve national or international environmental objectives. Challenges face this business in scaling the technology to reduce meaningfully the plan- et’s more than 250 000 000 dairy cattle and in formulating CM alternatives acceptable to children. One large plant under construction is estimated to be equivalent in some ways to 10 000 cows (see website cited in this paragraph). To replace 50% of the dairy cattle in the world would take 12 500 similar plants. Thus, the challenge of scaling this technology cannot be over-stated. In table 5, it can be seen that if these hurdles can be overcome, precision fermen- tation could offer alternatives to dairy milk that addresses many of the concerns leading to PBD development.
CONCLUSIONS
Nutritionally, many of today’s PBD do not provide the same nutrition as CM for young children. Soy beverages come nutritionally close to CM and are a reasonable alternative. Others, like most almond milks, fail to fill the dietary space of CM. Organic CM, fermented CM products and future beverages based on products of precision fermentation can be attractive, as they address some specific parental concerns. For the many parents who appear to feed their children PBD due to misconceptions about risks of CM and the nutritional value of PBD, better education and product labelling strategies are needed. The rationale for preferring plant based foods over animal foods, including milk, on the basis of fewer adverse environmental impacts and food supply sustainability has been well-established. The ethical perspective that we should not be eating
animals or causing them pain and suffering can be a deeply held personal view or religious tenet. For parents who exclude CM from the diet of their children on environmental or ethical grounds, better tasting alternative drinks for children that offer more complete nutrition with fewer additives and sugar will be welcome. PBD utilising more than one plant source have the potential to be more nutritionally complete with less fortification. To help those parents committed to feeding their children alternative drinks and to assure their children receive the nutrition they need, establishing a standard of identity and implementation of standard labelling for alternative child milk products could be helpful.
____________________________________
Acknowledgements. I thank Dr. Steven Schaefer for insightful comments on an early draft of this manuscript and Ms. Haydee Pampel for helpful editorial suggestions.
Contributors . All work in this manuscript was performed by the single author.
Funding. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests. Past Medical Director for Nestle USA and Abbott Laboratories. Retiree, Abbott Laboratories. Stockholder, Abbott Laboratories.
Patient consent for publication Not applicable.
Ethics approval Not applicable.
Provenance and peer review Commissioned; externally peer reviewed. Special issue - Annales Nestle - Foods for the future and their potential impact on child nutrition, by: Elvira Verduci, University of Milan, Italy; Diego Peroni, University of Pisa Faculty of Medicine and Surgery, Clinical Experimental Medicine, Italy.
REFERENCES
Singhal S, Baker RD, Baker SS. A comparison of the nutritional value of cow’s milk and nondairy beverages. J Pediatr Gastroenterol Nutr 2017;64:799–805.
Drewnowski A. Most plant-based milk alternatives in the USDA branded food products database do not meet proposed nutrient standards or score well on nutrient density metrics. Nutrients 2022;14:4767.
Verduci E, D’Elios S, Cerrato L, et al. Cow’s milk substitutes for children: nutritional aspects of milk from different mammalian species, special formula and plant-based beverages. Nutrients 2019;11:1739.
Vanga SK, Raghavan V. How well do plant based alternatives fare nutritionally compared to cow’s milk J Food Sci Technol 2018;55:10–20.
Smith NW, Dave AC, Hill JP, et al. Nutritional assessment of plant-based beverages in comparison to bovine milk. Front Nutr 2022;9:957486.
Merritt RJ, Fleet SE, Fifi A, et al. North American Society for pediatric gastroenterology, hepatology, and nutrition position paper: plant- based milks. J Pediatr Gastroenterol Nutr 2020;71:276–81.
Messina V, Reed Mangels A. Considerations in planning vegan diets: children. J Am Diet Assoc 2001;101:661–9.
Sutter DO, Bender N. Nutrient status and growth in vegan children. Nutr Res 2021;91:13–25.
Campion EW, Willett WC, Ludwig DS. Milk and health. N Engl J Med 2020;382:644–54.
McGovern C, Rifas-Shiman SL, Switkowski KM, et al. Association of cow’s milk intake in early childhood with adiposity and cardiometabolic risk in early adolescence. Am J Clin Nutr 2022;116:561–71.
Hojsak I, Bronsky J, Campoy C, et al. Young child formula: a position paper by the ESPGHAN Committee on nutrition. J Pediatr Gastroenterol Nutr 2018;66:177–85.
J MR. Pediatric nutrition 8th edition. In: Kleinman RG, ed. Formula Feeding of Term Infants. Itasca, Il: American Academy of Pediatrics, 2019: 79–112.
Attia SL, Fuchs GJ. Toddler formula, young child formula, growing up milk: the wild west of young child nutrition. J Pediatr Gastroenterol Nutr 2023;76:401.
Du N, DiMaggio DM, Porto AF. Nutrition content of young child formulas. J Pediatr Gastroenterol Nutr 2023;76:512–6.
Hoppe C, Mølgaard C, Michaelsen KF. Cow’s milk and linear growth in industrialized and developing countries. Annu Rev Nutr 2006;26:131–73.
Morency M-E, Birken CS, Lebovic G, et al. Association between noncow milk beverage consumption and childhood height. Am J Clin Nutr 2017;106:597–602.
Steinman H. Implications of food allergies. South African Journal of Clinical Nutrition 2010;23:37–41.
Mehta H, Ramesh M, Feuille E, et al. Growth comparison in children with and without food allergies in 2 different demographic populations. J Pediatr 2014;165:842–8.
Grenov B, Larnkjær A, Ritz C, et al. The effect of milk and rapeseed protein on growth factors in 7-8 year-old healthy children - a randomized controlled trial. Growth Horm IGF Res 2021;60–61:101418.
van Stuijvenberg ME, Nel J, Schoeman SE, et al. Low intake of calcium and vitamin D, but not zinc, iron or vitamin A, is associated with stunting in 2- to 5-year-old children. Nutrition 2015;31:841–6.
Grasgruber P, Sebera M, Hrazdíra E, et al. Major correlates of male height: a study of 105 countries. Econ Hum Biol 2016;21:172–95.
Singhal A. Long-term adverse effects of early growth acceleration or catch-up growth. Ann Nutr Metab 2017;70:236–40.
Flom JD, Sicherer SH. Epidemiology of cow’s milk allergy. Nutrients 2019;11:1051.
Koletzko S, Niggemann B, Arato A, et al. Diagnostic approach and management of cow’s-milk protein allergy in infants and children: ESPGHAN GI committee practical guidelines. J Pediatr Gastroenterol Nutr 2012;55:221–9.
Storhaug CL, Fosse SK, Fadnes LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2017;2:738–46.
Thorning TK, Raben A, Tholstrup T, et al. Milk and dairy products: good or bad for human health? An assessment of the totality of scientific evidence. Food Nutr Res 2016;60:32527.
Wong VCH, Maguire JL, Omand JA, et al. A positive association between dietary intake of higher cow’s milk-fat percentage and non-high-density lipoprotein cholesterol in young children. J Pediatr 2019;211:S0022-3476(19)30408-1:105–111..
Melnik BC. Lifetime impact of cow’s milk on overactivation of mTORC1: from fetal to childhood overgrowth, acne, diabetes, cancers, and neurodegeneration. Biomolecules 2021;11:404.
Calahorrano-Moreno MB, Ordoñez-Bailon JJ, Baquerizo-Crespo RJ, et al. Contaminants in the cow’s milk we consume? Pasteurization and other technologies in the elimination of contaminants. F1000Res 2022;11:91.
Welsh JA, Braun H, Brown N, et al. Production-related contaminants (pesticides, antibiotics and hormones) in organic and conventionally produced milk samples sold in the USA. Public Health Nutr 2019;22:2972–80.
Kosgey A, Shitandi A, Marion JW. Antibiotic residues in milk from three popular Kenyan milk vending machines. Am J Trop Med Hyg 2018;98:1520–2.
Kurjogi M, Issa Mohammad YH, Alghamdi S, et al. Detection and determination of stability of the antibiotic residues in cow’s milk. PLoS One 2019;14:e0223475.
Groenewegen PP, McBride BW, Burton JH, et al. Bioactivity of milk from bST-treated cows. J Nutr 1990;120:514–20.
Hoeflich A, Meyer Z. Functional analysis of the IGF-system in milk. Best Pract Res Clin Endocrinol Metab 2017;31:409–18.
Maruyama K, Oshima T, Ohyama K. Exposure to exogenous estrogen through intake of commercial milk produced from pregnant cows. Pediatr Int 2010;52:33–8. 10.1111/j.1442-200X.2009.02890.x Available: http://blackwell-synergy.com/doi/abs/10.1111/ped.2010. 52.issue-1
McClements DJ, Newman E, McClements IF. Plant‐based milks: a review of the science underpinning their design, fabrication, and performance. Compr Rev Food Sci Food Saf 2019;18:2047–67.
Petroski W, Minich DM. “Is there such a thing as “anti-nutrients”? A narrative review of perceived problematic plant compounds”. Nutrients 2020;12:2929.
Coluccia B, Agnusdei GP, De Leo F, et al. Assessing the carbon footprint across the supply chain: cow milk vs soy drink. Sci Total Environ 2022;806(Pt 3):151200.
Drewnowski A. Perspective: identifying ultra-processed plant-based milk alternatives in the USDA branded food products database. Adv Nutr 2021;12:2068–75.
Monteiro CA, Cannon G, Moubarac JC, et al. The UN decade of nutrition, the NOVA food classification and the trouble with ultra- processing. Public Health Nutr 2018;21:5–17.
Wang L, Martínez Steele E, Du M, et al. Trends in consumption of ultraprocessed foods among US youths aged 2-19 years, 1999- 2018. JAMA 2021;326:519.
Kelly B, Jacoby E. Public health nutrition special issue on ultra- processed foods. Public Health Nutr 2018;21:1–4.
Meek JY, Noble L. Section on breastfeeding. Policy statement: breastfeeding and the use of human milk. Pediatrics 2022;150:e2022057988.
Siega-Riz AM, Deming DM, Reidy KC, et al. Food consumption patterns of infants and toddlers: where are we now J Am Diet Assoc 2010;110:S38–51.
Bhatia J, Greer F. American academy of pediatrics committee on nutrition. use of soy protein-based formulas in infant feeding. Pediatrics 2008;121:1062–8.
Suen AA, Kenan AC, Williams CJ. Developmental exposure to phytoestrogens found in soy: new findings and clinical implications. Biochem Pharmacol 2022;195:114848.
Merritt RJ, Jenks BH. Safety of soy-based infant formulas containing isoflavones: the clinical evidence. J Nutr 2004;134:1220S–1224S.
Dupont C, Bocquet A, Tomé D, et al. Hydrolyzed rice protein-based formulas, a vegetal alternative in cow’s milk allergy. Nutrients 2020;12:2654.
Vitoria I. The nutritional limitations of plant-based beverages in infancy and childhood. Nutr Hosp 2017;34:1205–14.
Cifelli CJ, Houchins JA, Demmer E, et al. Increasing plant based foods or dairy foods differentially affects nutrient intakes: dietary scenarios using NHANES 2007–2010. Nutrients 2016;8:422.
Desmond MA, Sobiecki JG, Jaworski M, et al. Growth, body composition, and cardiovascular and nutritional risk of 5- to 10-Y-old children consuming vegetarian, vegan, or omnivore diets. Am J Clin Nutr 2021;113:1565–77.
Escobar-Sáez D, Montero-Jiménez L, García-Herrera P, et al. Plant- based drinks for vegetarian or vegan toddlers: nutritional evaluation of commercial products, and review of health benefits and potential concerns. Food Res Int 2022;160:111646.
Haas R, Schnepps A, Pichler A, et al. Cow milk versus plant-based milk substitutes: a comparison of product image and motivational structure of consumption. Sustainability 2019;11:5046.
Beck V, Ladwig B. Ethical consumerism: veganism. WIREs Clim Change 2021;12:e689. 10.1002/wcc.689 Available: https://onlinelibrary.wiley.com/ toc/17577799/12/1
Beauchemin KA, Ungerfeld EM, Eckard RJ, et al. Review: fifty years of research on rumen methanogenesis: lessons learned and future challenges for mitigation. Animal 2020;14:s2–16.
Alae-Carew C, Green R, Stewart C, et al. The role of plant- based alternative foods in sustainable and healthy food systems: consumption trends in the UK. Sci Total Environ 2022;807(Pt 3):151041.
Poore J, Nemecek T. Reducing food’s environmental impacts through producers and consumers. Science 2018;360:987–92.
Schiano AN, Harwood WS, Gerard PD, et al. Consumer perception of the sustainability of dairy products and plant-based dairy alternatives. J Dairy Sci 2020;103:11228–43.
Fifi AC, Pagan DN, Chakraborty P, et al. Physician and parent perceptions on plant-based beverages as substitutes for cow’s milk: a single city survey. J Pediatr Gastroenterol Nutr 2022;75:e25–9.
Laila A, Topakas N, Farr E, et al. Barriers and facilitators of household provision of dairy and plant-based dairy alternatives in families with preschool-age children. Public Health Nutr 2021;24:5673–85.
Aro N, Ercili-Cura D, Andberg M, et al. Production of bovine beta- lactoglobulin and hen egg ovalbumin by trichoderma reesei using precision fermentation technology and testing of their techno-functional properties. Food Res Int 2023;163:112131.
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific opinion on the essential composition of infant and follow- on formulae. EFSA Journal 2014;12:3760.