Nutritional Strategies to Prevent Preterm Birth
Key messages:
- An estimated 10% of babies worldwide are born preterm with much higher incidence in Africa and South Asia.1
- Current preventative strategies and interventions only work for a specific subset of women due to heterogeneity in outcomes and a lack of understanding of the underlying mechanisms.
- Nutritional strategies to prevent preterm birth are a promising approach with a growing body of clinical evidence. Recent intervention studies support a role for omega-3 and of micronutrients in reducing the risk of preterm birth.
The occurrence of preterm births have gone up to roughly 10% of babies globally. With current means of prevention being partial to a specific subset of women, cases occur much higher in certain regions, such as in Africa and South Asia. Nutritional strategies for preterm birth prevention are now being tapped, especially with the growing support from more and more clinical studies, specifically the use of omega-3 and micronutrients.
Key messages:
- An estimated 10% of babies worldwide are born preterm with much higher incidence in Africa and South Asia.1
- Current preventative strategies and interventions only work for a specific subset of women due to heterogeneity in outcomes and a lack of understanding of the underlying mechanisms.
- Nutritional strategies to prevent preterm birth are a promising approach with a growing body of clinical evidence. Recent intervention studies support a role for omega-3 and of micronutrients in reducing the risk of preterm birth.
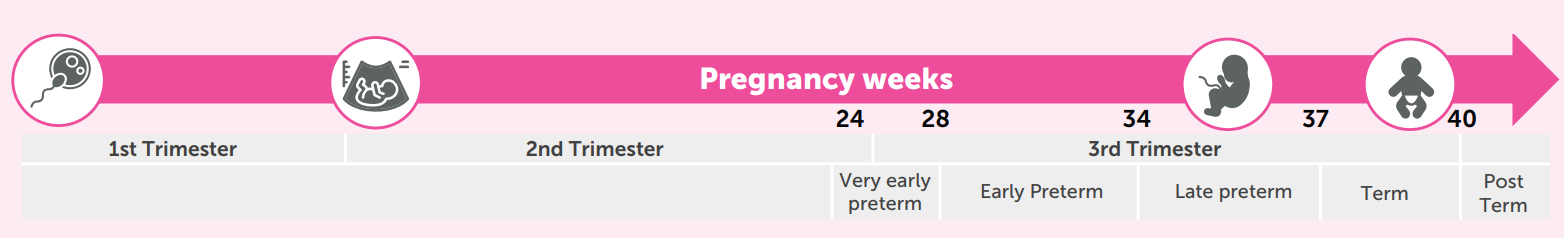
Preterm birth (PTB) is defined as any birth before 37 completed weeks of gestation (FIG.1.). Every year, 15 million babies are born preterm globally. PTB is the leading cause of mortality among children below the age of five. While advances in medical care have improved the survival rate of babies born preterm, it can lead to short and long-term adverse health outcomes.
Risk factors of preterm birth
The causes and mechanisms of PTB are not well established. Most PTBs happen spontaneously, however, several risk factors have been identified. Some of these risk factors are non-modifiable while others like diet and lifestyle risk factors can be addressed (FIG.2.). To-date, very few interventions exist that can effectively reduce the risk of PTB. The interventions that do exist are mainly the use of pharmaceuticals (progesterone, tocolytics) or medical procedures such as cervical cerclage or insertion of a pessary. However, these are effective only in specific groups of women1,2 and require early screening for risk factors, recognition of high risk and decision to intervene, as well as close medical monitoring.
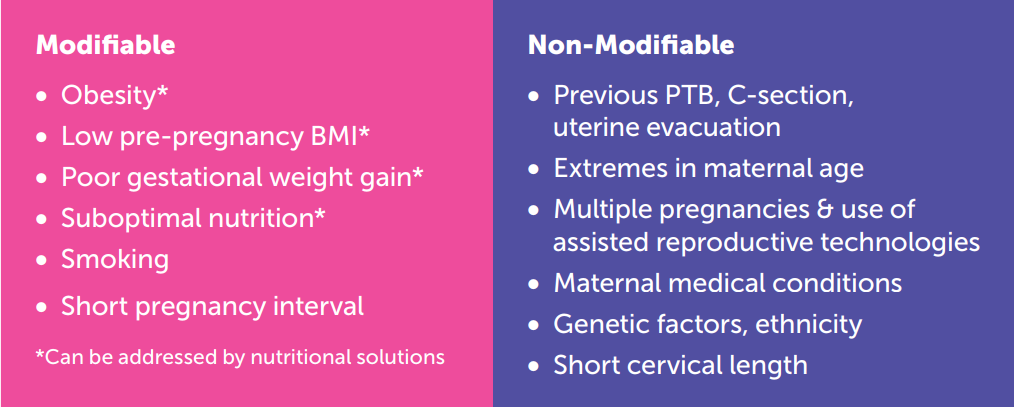
Nutritional solutions are a promising avenue to reduce PTB risk. They can address various risk factors such as suboptimal nutrition, suboptimal BMI, poor gestational weight gain and (gestational) diabetes.2 Omega-3 fatty acids (DHA and EPA) have the highest strength of evidence to reduce PTB risk.3 Other nutrients, albeit with varying levels of evidence, have also been reported to modulate PTB risk. These include zinc, vitamin D, vitamin A, calcium, iron, folic acid, combined iron-folate, magnesium and probiotics.2
Nutritional intervention trials
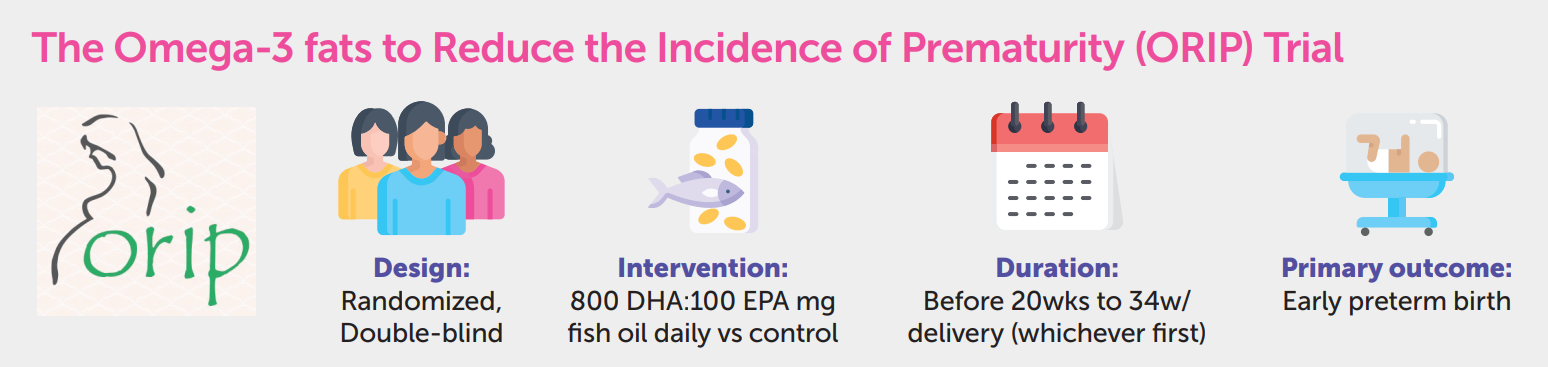
Two large clinical studies provide strong support for the role of omega-3 intervention to reduce the risk of PTB. The ORIP (Omega-3 Fats to Reduce the Incidence of Prematurity) study supplemented pregnant women with 900 mg/day of omega-3 LCPUFA (DHA:EPA 8:1) from 20 to 34 weeks of gestation (FIG.3.). Results indicated that women with low baseline omega-3 status in early pregnancy had lower relative risk of early preterm birth when supplemented with this high dose of omega-3.4 However, the same analysis also suggested that high dose omega-3 supplementation increased the relative risk of early preterm birth in women with already high omega-3 status at baseline. Similarly, findings from the ADORE (Assessment of DHA on reducing early preterm birth) clinical study indicate that that women with low baseline omega-3 status benefit the most from high dose DHA (1000mg) supplementation during pregnancy.5
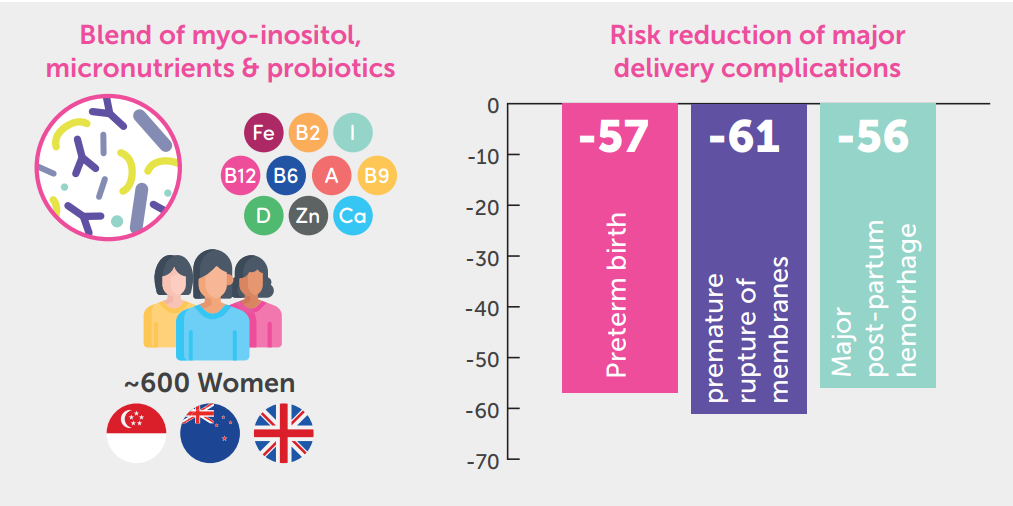
While there is emerging evidence to suggest a positive impact of multiple micronutrient (MMN) supplementation in reducing the risk of PTB, this seems limited to low- and middle-income countries.6 However, recent findings from a clinical trial with an enriched nutritional formulation showed promising results. The Nutritional Intervention Preconception and During Pregnancy to Maintain Healthy Glucose Metabolism and Offspring Health (NiPPeR) trial compared a nutritional formulation containing myo-inositol, probiotics and MMN with a standard micronutrient supplement on pregnancy outcomes. The study findings indicated a reduced incidence of PTB in the intervention group. The effect was particularly observed for late PTB (34-36 gestational weeks) and was associated with lower preterm pre-labor rupture of membranes (FIG.4).7
Results from these recent clinical studies reinforce the relevance of nutritional intervention strategies to reduce the risk of PTB. Although mostly conducted in affluent populations, these strategies can potentially target a variety of mechanisms that contribute to PTB and may prove to be a highly effective preventative approach.
References
- WHO Factsheet-Preterm birth: https://www.who. int/news-room/fact-sheets/detail/preterm-birth
- Samuel TM, Sakwinska O, Makinen K, Burdge GC, Godfrey KM, Silva-Zolezzi I. Preterm Birth: A Narrative Review of the Current Evidence on Nutritional and Bioactive Solutions for Risk Reduction. Nutrients. 2019 Aug 6;11(8):1811. doi: 10.3390/nu11081811. PMID: 31390765; PMCID: PMC6723114.
- Middleton P, Gomersall JC, Gould JF, Shepherd E, Olsen SF, Makrides M. Omega-3 fatty acid addition during pregnancy. Cochrane Database Syst Rev. 2018 Nov 15;11(11):CD003402. doi: 10.1002/14651858.CD003402.pub3. PMID: 30480773; PMCID: PMC6516961.
- Simmonds LA, Sullivan TR, Skubisz M, Middleton PF, Best KP, Yelland LN, Quinlivan J, Zhou SJ, Liu G, McPhee AJ, Gibson RA, Makrides M. Omega-3 fatty acid supplementation in pregnancybaseline omega-3 status and early preterm birth: exploratory analysis of a randomised controlled trial. BJOG. 2020 Jul;127(8):975-981. doi: 10.1111/1471-0528.16168. Epub 2020 Mar 3. PMID: 32034969.
- Carlson, S. E., Gajewski, B. J., Valentine, C. J., Kerling, E. H., Weiner, C. P., Cackovic, M., DeFranco, E. A. (2021). Higher dose docosahexaenoic acid supplementation during pregnancy and early preterm birth: A randomised, double-blind, adaptive-design superiority trial. eClinicalMedicine, 36. doi:10.1016/j.eclinm.2021.100905.
- Keats EC, Haider BA, Tam E, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019 Mar 14;3(3):CD004905. doi: 10.1002/14651858.CD004905.pub6. PMID: 30873598; PMCID: PMC6418471.
- Godfrey, K. M., Barton, S. J., El-Heis, S., Kenealy, T., Nield, H., Baker, P. N., Chong, Y. S., Cutfield, W., Chan, S. Y., & NiPPeR Study Group (2021). Myo-Inositol, Probiotics, and Micronutrient Supplementation From Preconception for Glycemia in Pregnancy: NiPPeR International Multicenter Double-Blind Randomized Controlled Trial. Diabetes care, 44(5), 1091–1099. https://doi.org/10.2337/dc20-2515

