Epidemiology of Mastitis
Epidemiology of Mastitis
Gillian A. Ryan and Chittaranjan N. Purandare
Key Messages
- Mastitis is one of the most common problems encountered by the breastfeeding mother
- Many women stop breastfeeding due to mastitis or breast abscesses
- Prevention of mastitis is very important in supporting of breastfeeding
Breastfeeding and lactation are an integral part of reproductive physiology. Breastfeeding is recommended as the exclusive source of nutrition for infants in the first 6 months of life by many international bodies, including the American College of Obstetricians and Gynecologists, WHO, and FIGO. Furthermore, continued breastfeeding is recommended along with appropriate complementary foods up to two years of age or beyond [1, 2]. However, many women stop breastfeeding due to mastitis or breast abscesses. As obstetricians, it is important that we not only support breastfeeding mothers to achieve successful breastfeeding but also that we should be aware of the common complications that can occur as a result of breastfeeding and the most appropriate management of these conditions. This is important for the health and well-being of both the mother and the child, but also as women who experience breastfeeding difficulties are at higher risk of postpartum depression, and should be screened, treated, and referred appropriately [1].
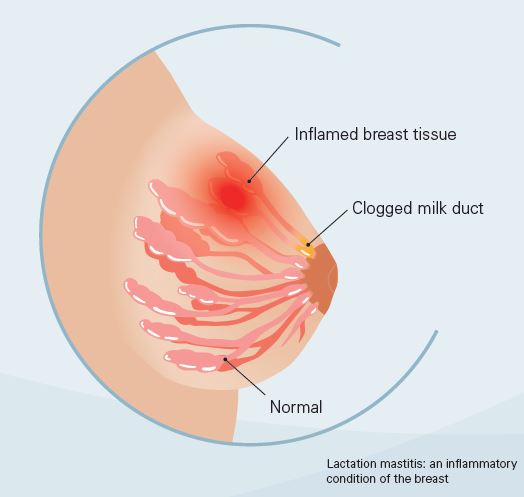
Mastitis is one of the most common problems encountered by the breastfeeding mother. It is an inflammatory condition of the breast and may occur with or without infection. It is also commonly termed lactational mastitis or puerperal mastitis. Lactational mas-titis has been estimated to occur in approximately 2–10% of all breastfeeding women [3, 4], though the reported incidence varies from one population to another, with some studies quoting rates as high as 30% [4]. The most common time of occurrence of masti-tis is in the second or third week postpartum [4]. The development of a breast abscess is a severe complication of mastitis. This is a localized collection of pus within the breast, and the incidence is approximately 0.1–3% [5, 6]. The occurrence of a breast abscess is also commonest in the first 6 weeks postpartum, but may also occur later [4], and it can occur with or without preceding mastitis.
The incidence of mastitis requiring hospitalization is low; one study by Stafford et al. [7] included 136,459 new mothers, and found 127 women required hospitalization for mastitis, which resulted in an incidence of 9 per 10,000 deliveries. Although generally easily treatable with antibiotics, it can occasionally be fatal if inadequately treated. Research suggests that mastitis also increases the risk of transmission of HIV to the infant through breastfeeding [8]. Although complications can occur, it is typically easily treated with antibiotics; and with the appropriate support and education, breastfeeding can be continued.
References
- American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice; Breastfeeding Expert Work Group: Committee Opinion No. 658 Summary: optimizing support for breastfeeding as part of obstetric practice. Obstet Gynecol 2016;127:420–421.
- WHO: Breastfeeding. http://www.who.int/ topics/breastfeeding/en/
- Committee on Health Care for Underserved Women, American College of Obstetricians and Gynecologists: ACOG Committee Opinion No. 361: breastfeeding: maternal and infant aspects. Obstet Gynecol 2007;109:479–480.
- Department of Child and Adolescent Health and Development, World Health Organization: Mastitis – Causes and Management. Geneva, World Health Organization, 2000.
- Dener C, Inan A: Breast abscesses in lactating women. World J Surg 2003;27:130.
- Amir LH, Forster D, McLachlan H, Lumley J: Incidence of breast abscess in lactating women: report from an Australian cohort. BJOG 2004;111:1378.
- Stafford I, Hernandez J, Laibl V, Sheffield J, Roberts S, Wendel G Jr: Community-acquired methicillin-resistant Staphylococcus aureus among patients with puerperal mastitis requiring hospitalization. Obstet Gynecol 2008;112:533–537.
- Semrau K, Kuhn L, Brooks DR, Cabral H, SinkalaM, Kankasa C, Thea DM, Aldrovandi GM: Dynamics of breast milk HIV-1 RNA with unilateral mastitis or abscess. J Acquir Immune Defic Syndr 2013;62:348–355.